Call Us
by Adam Brown
Registered Physiotherapist
updated Oct 8, 2020
What is Plantar Fasciitis?
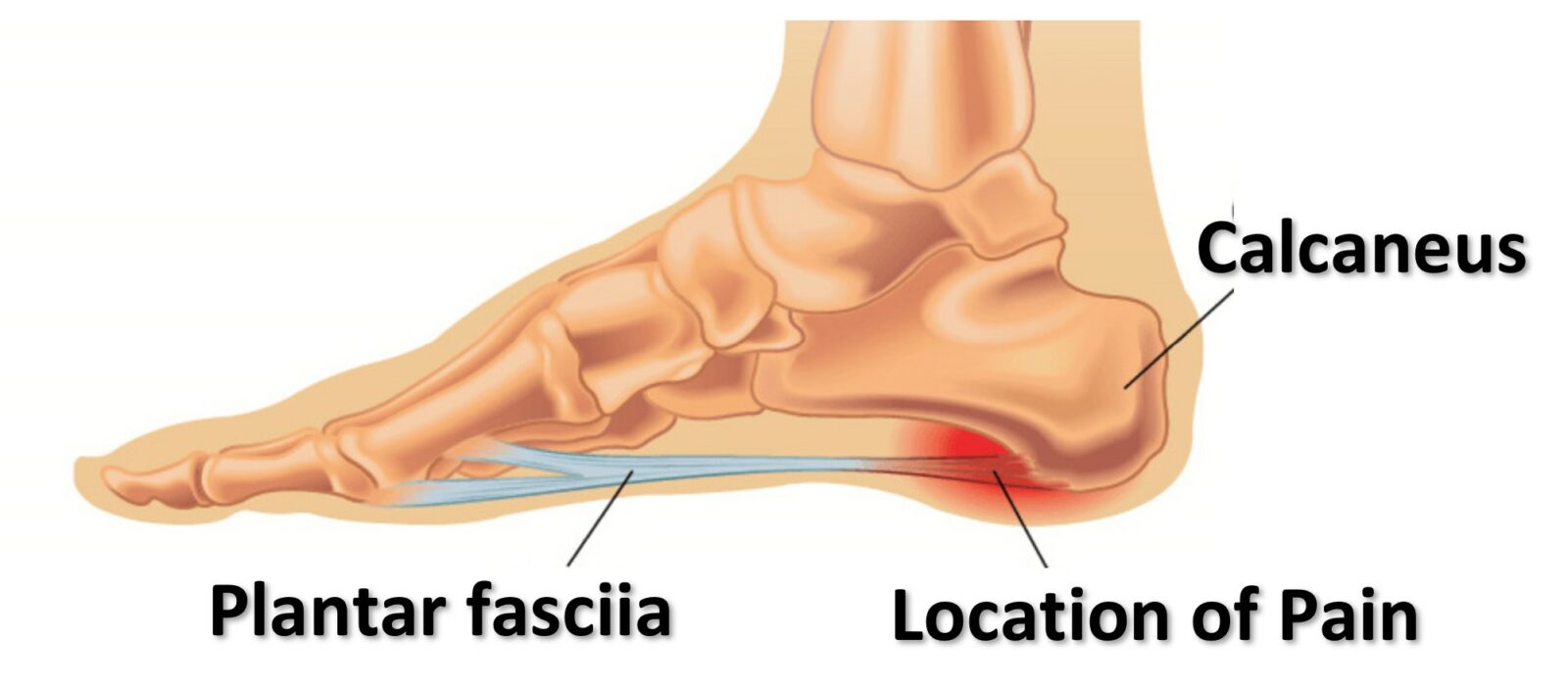
Plantar Fasciitis is the leading cause of foot pain and is a difficult problem to resolve. It is characterized by breakdown and inflammation of the plantar fascia, a strong band of tissue on the bottom of your foot that connects your heel to your toes. The plantar fascia comes under tension when you stand or walk. It’s function is to assist the joints of your foot and ankle to absorb force and maintain good lower extremity alignment. But like any tissue in the body, if the strain on your plantar fascia increases faster than your body can adapt, breakdown of that tissue will follow.
Most patients report a stabbing pain in the heel where the plantar fascia meets the heel bone (or calcaneous) on the underside of the foot. Usually people feel intense pain on the first few steps after they wake up in the morning, or after sitting for long periods. Pain is reduced after walking a short distance, and will increase again after prolonged standing and walking.
What Causes Plantar Fasciitis?
There is no single cause that is common for all cases of plantar fasciitis, but there are some common patterns that create conditions where the strain on the tissue exceeds the bodies ability to adapt. At any given time, your plantar fascia is as strong and resilient as it needs to be to meet the demands of your recent physical activity. If your activity increases slowly and with adequate rest time, the tissue will become thicker, stronger and will remain healthy and pain free. However if strain increases at a rate that the body can not keep up with, it leads to failure of the plantar fascia. This usually takes the form of very small tears in the tissue causing pain and inflammation.
Some risk factors for developing plantar fasciitis are;
- Age – middle aged (between 40 and 60 years) people tend to develop this condition more.
- Gender – More women suffer from plantar fasciitis than men.
- Foot type – people with flatter feet or very high arches are at higher risk.
- Body Weight – the heavier you are, the more strain you place on your feet with each step.
- Your Job – If you work on your feet all day, especially on hard surfaces with poor footwear, your risk increases.
- Sport – distance runners are at higher risk – especially if they ramp their mileage up too quickly.
- Other Injuries – After an extended period of non weight bearing due to injury or illness (such as being on crutches) activity must be resumed carefully to avoid overloading weakened tissue.
How is Plantar Fasciitis Diagnosed?
Diagnosis is made with a simple history and physical exam. Heel pain that is worst in the morning or after prolonged sitting that tends to get better after some movement, coupled with tenderness at the insertion of the plantar fascia is indicative of plantar fasciitis.
Imaging like an x-ray or bone scan are not typically required to make an accurate diagnosis, but may be used to rule out other conditions such as stress fractures.
An x-ray will often reveal a bone spur on the heel. While we used to think these heel spurs were a cause of pain, we now understand that they are simply an adaptation of the bone to increased tension on the fascia. Many people have bone spurs on an x-ray but have no heel pain at all.
There are a few other conditions that cause foot and ankle pain (see below) so it is important to have an experienced physiotherapist or sports medicine physician examine the problem to ensure you have the correct diagnosis before creating a treatment plan.
Why Does Plantar Fasciitis Hurt in The Morning?
Almost everyone with plantar fasciitis dreads their first few steps in the morning. They experience stabbing pain in the heel on each step that tends to subside as they walk more. There are two reasons that this happens.
First, blood flow through the plantar fascia is assisted when the tissue is placed under tension and released repetitively (such as walking). Imagine a rope that is wet. When you pull on the rope, water leaks out, and when you release tension water can be reabsorbed. When you are sleeping there is no tension on the plantar fascia for an extended period of time. This means that some of the inflammation will not be flushed away by the circulatory system as efficiently, leading to more sensitivity.
Second, and perhaps more importantly, your foot and ankle are typically pointed (or plantar flexed) when you are sleeping. This is a shortened position for the plantar fascia as well as your calf muscles which are connected to the fascia. When you stand up in the morning you are rapidly lengthening the tissue under the force of your entire body weight. What seems like a simple step to you, is a big stretch under a great deal of force for your plantar fascia, resulting in pain.
A good strategy is to do a simple gentle stretch for a few minutes before getting out of bed. Here are two options for stretching your plantar fascia in the morning to reduce the pain on your first steps.


Will My Plantar Fasciitis Go Away?
Plantar fasciitis can be a chronic problem and for most people it will take several months to completely resolve with treatment. If the condition is left untreated it can go on for a very long time. As a physiotherapist it is not uncommon to encounter patients that have been dealing with some form of plantar fasciitis for several years before they seek proper treatment.
Treatment For Plantar Fasciitis?
The key to effective therapy for plantar fasciitis is to recognize what stage of healing the condition is in, and tailor treatment to promote repair.
Acute Plantar Fasciitis
When the condition is new, it is particularly painful and is marked by a high degree of inflammation. At this stage it is important to reduce stress on the tissue to give the inflammatory response a chance to resolve.
Some good treatment strategies for acute plantar fasciitis are;
- Rest
- Ice
- Gentle stretching of the calves and plantar fascia.
- Changing to footwear with good arch support.
- Consider foot orthotics (shoe inserts) to reduce force on the tissue while walking.
- Use of a cane or crutch for a short duration in particularly painful cases.
- Anti-inflammatory medications like Ibuprofen.
- Reduction of stress from sport or occupational hazards.
Chronic Plantar Fasciitis
Most patients we see in the physiotherapy clinic have chronic plantar fasciitis. Their condition has improved since the acute stage, but has become stuck in the chronic stage preventing them from walking comfortably or participating in their usual sport or work activities. it requires an experienced and skilled therapist to recognize the causes of excessive force on the fascia and to design a treatment plan that will stimulate the tissue to thicken and recover without creating further injury.
Some good treatment strategies used for chronic plantar fasciitis are;
- Correction of training errors to ensure an appropriate amount of stress on the tissue and adequate recovery time.
- Change in footwear – particularly for runners or people who work while standing all day.
- Some patients benefit from foot orthotics to reduce strain on the fascia. For an explanation of how orthotics work click HERE
- Night splints can help maintain the fascia and calves in a lengthened position while sleeping, reducing pain and tightness in the first half of the day.
- Load management – exercises to apply appropriate stress to the tissue to stimulate chan
ge followed by a rest period to allow for recovery.
- Strength – in particular the flexor hallucis longus and tibialis posterior muscles must be strong to support the arch of the foot and reduce strain on the plantar fascia.
- Mobility – if the ankle is stiff it can lead to excessive mid-foot pronation and increased stress on the plantar fascia. In this case manual therapy and exercises to restore good ankle mobility will be necessary for recovery.
- Hip/Core strength and control – poor control of the lower extremity from above causes the leg to internally rotate and the arch of the foot to collapse placing increased stress on the plantar fascia.
- Stretching – Calf and plantar fascia stretches can help to ensure that the new tissue becomes adequately mobile and strong.
- Shockwave Therapy (extracorporeal shockwave therapy) – Has been shown to stimulate healing in the plantar fascia.
Stubborn Chronic Plantar Fasciitis
A very small number of patients will not be bale to resolve their plantar fasciitis despite months of participation in a sensible rehabilitation program. For these individuals further medical management may be required.
Some treatments available for plantar fasciitis that has not responded to usual treatment are;
- Injections – Cortisone injections can provide short term pain relief and some evidence suggests that Platelet Rich Plasma (PRP) injections may help stimulate healing in otherwise stubborn tissue.
- Surgery – in extreme cases patients undergo a release of the plantar fascia. This is a treatment of last resort because the plantar fascia has an important role to play in the proper function of the foot. For a brief video showing a plantar fascia release surgery click HERE
What Other Problems Cause Foot Pain?
The plantar fascia is the most common cause of heel pain but it is certainly not the only cause. Here is a list of conditions that are capable of creating heel pain and a few notes on how to tell them apart form plantar fasciitis.
Tarsal Tunnel Syndrome

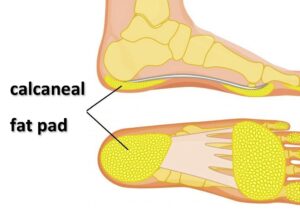
Calcaneal Fat Pad Syndrome
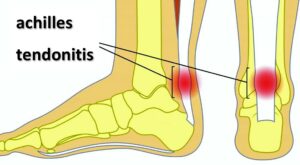
Achilles Tendonitis
Stress Fracture
Stress fractures are small non-displaced fractures of bone due to repetitive overload. They are discovered on a bone scan or if they have been healing for more than a few weeks may be visible on an x-ray. The pain related to a stress fracture does not improve with gentle activity making it distinct from that of a tendonitis or plantar fasciitis.
Final thoughts on Plantar Fasciitis
Typically patients initially underestimate how difficult it will be to resolve their plantar fasciitis. While the condition is not serious or life threatening, it can certainly prevent you from getting appropriate physical activity resulting in poor fitness and a significant decline in quality of life. In you are dealing with plantar fasciitis take the following steps immediately;
- Get assessed by an experienced orthopaedic physical therapist and get a treatment plan started.
- Review your footwear to ensure that you have appropriate support (watch the video below).
- Reduce strain on the tissue as required and provide adequate rest for the tissue to heal between stressful events/treatments.
- Consider the addition of an orthotic and shockwave therapy if appropriate to your case.
- Discover strength and mobility deficits that are placing increased stress on the fascia and ensure your physical therapy plan is correcting them.
If you take the condition seriously, and you are diligent with your treatment plan you will be successful in eliminating your plantar fasciitis.

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749





 ge followed by a rest period to allow for recovery.
ge followed by a rest period to allow for recovery.