Call Us
Melissa Seifried MScPT
Registered Physiotherapist
Director of Long COVID Rehabilitation
updated Mar 6, 2024
Mast Cell Activation Syndrome (MCAS) is a condition that can affect both children and adults, forming part of a spectrum of mast cell disorders. In 2021, an observational study concluded that mast cell activation symptoms were increased in individuals suffering from Long COVID and mimicked the symptoms and severity reported by patients who have MCAS.1 By early 2023, follow up studies agreed with these observations.2,3
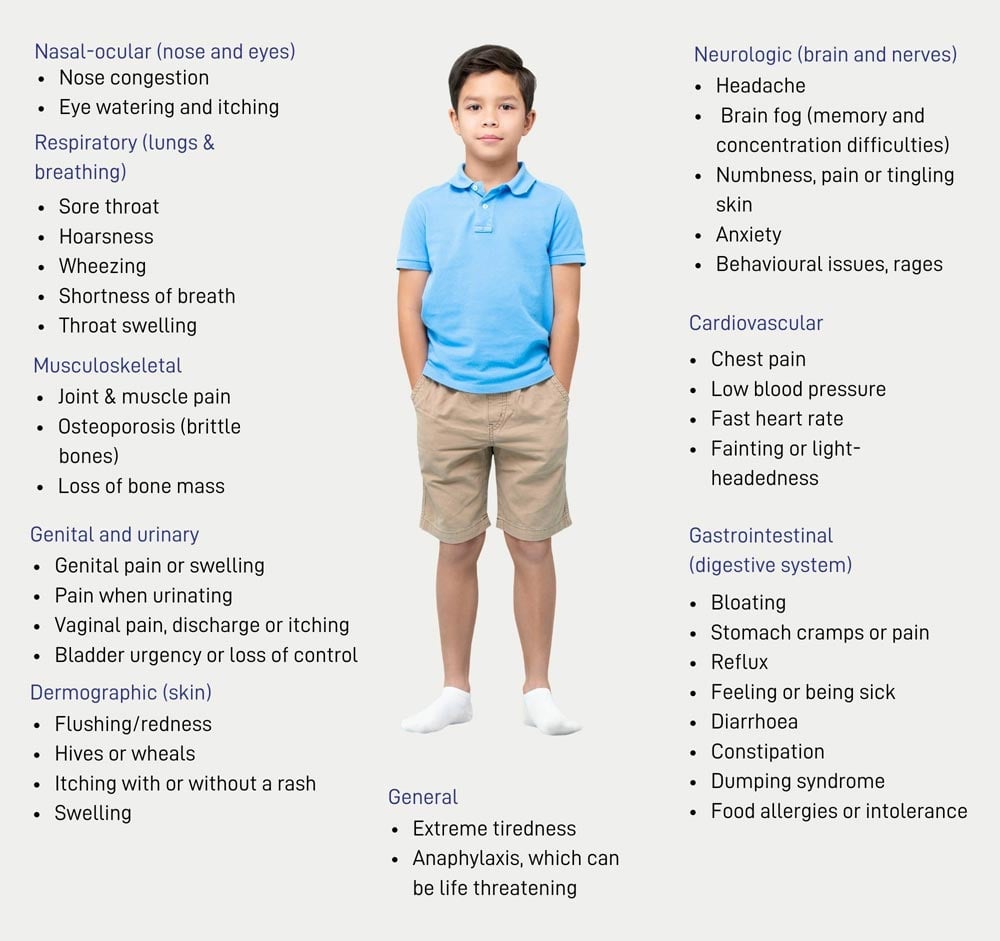
In MCAS, the body releases mast cell mediators excessively or in response to triggers that are not typically harmful, such as certain foods or environmental chemicals. This overreaction can result in a diverse range of symptoms affecting various systems in the body including the cardiopulmonary, gastrointestinal, dermatological, and neurological systems.
What Are Mast Cells?
Mast cells are a type of blood cell crucial to the body’s immune system. They act as the “police officers” of the immune system, detecting triggers and instructing other immune cells on how to respond. In a healthy state, mast cell mediators help fight infections and promote healing. However, in MCAS, the release of these mediators occurs too frequently, leading to multiple symptoms in different parts of the body simultaneously.
How is MCAS Diagnosed?
Diagnosing MCAS can be a complex process, involving four stages recommended by published guidance:4
Stage 1: Recognizing multi-systemic symptoms during a reaction, as no two individuals experience MCAS in exactly the same way.
Stage 2: Determining if symptoms improve with specific medications, indicating a potential diagnosis.
Stage 3: Conducting tests to identify elevated levels of chemical mediators in the blood or urine.
Stage 4: Eliminating other possible causes of symptoms, ensuring a thorough diagnostic process to exclude overlapping conditions.
What are the Common Symptoms of MCAS?
(https://www.mastcellaction.org/mcas-symptoms)
Anaphylaxis and Comorbidities
Individuals with MCAS are at an increased risk of experiencing anaphylactic reactions, which are potentially life-threatening allergic responses. Pre-loaded adrenaline auto-injectors, like EpiPens, are prescribed to counteract anaphylaxis.
Common comorbidities associated with MCAS include connective tissue disorders like Ehlers Danlos Syndrome (EDS), dysautonomia including Postural Orthostatic Tachycardia Syndrome (POTS), and Type 2 Diabetes. The relationship between MCAS and these conditions requires further research.
Identifying Triggers and Dietary Considerations
Triggers for MCAS can vary widely among individuals and may include fragrances, exercise, stress, temperature changes, and certain foods. Keeping a diary can help identify patterns and common themes, aiding in trigger recognition.
Dietary considerations play a significant role in managing MCAS, with elimination diets, guided by a Registered Dietitian, being commonly used. These diets may include low histamine, dairy-free, gluten-free, low salicylates, low oxalates, low FODMAP, low sugar (ketogenic), or a combination of any of these.
Managing MCAS
While there is currently no cure for MCAS, treatment aims to reduce symptom severity and improve quality of life. The two main approaches for symptom management are self-management and medical interventions.
Self-Management
Avoiding known food triggers, including specific diets like low histamine or FODMAPS.
Managing the personal environment to eliminate common triggers like scented products.
Identifying and avoiding medications that may trigger MCAS symptoms including medications with codeine. Some individuals with MCAS also benefit from avoiding non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen.
Understanding and managing individual triggers can provide significant relief for many individuals with MCAS, though it may not always be practical to avoid every trigger in all situations. Seeking guidance from healthcare professionals like your primary care physician and a Registered Dietitian is crucial in developing effective self-management strategies.
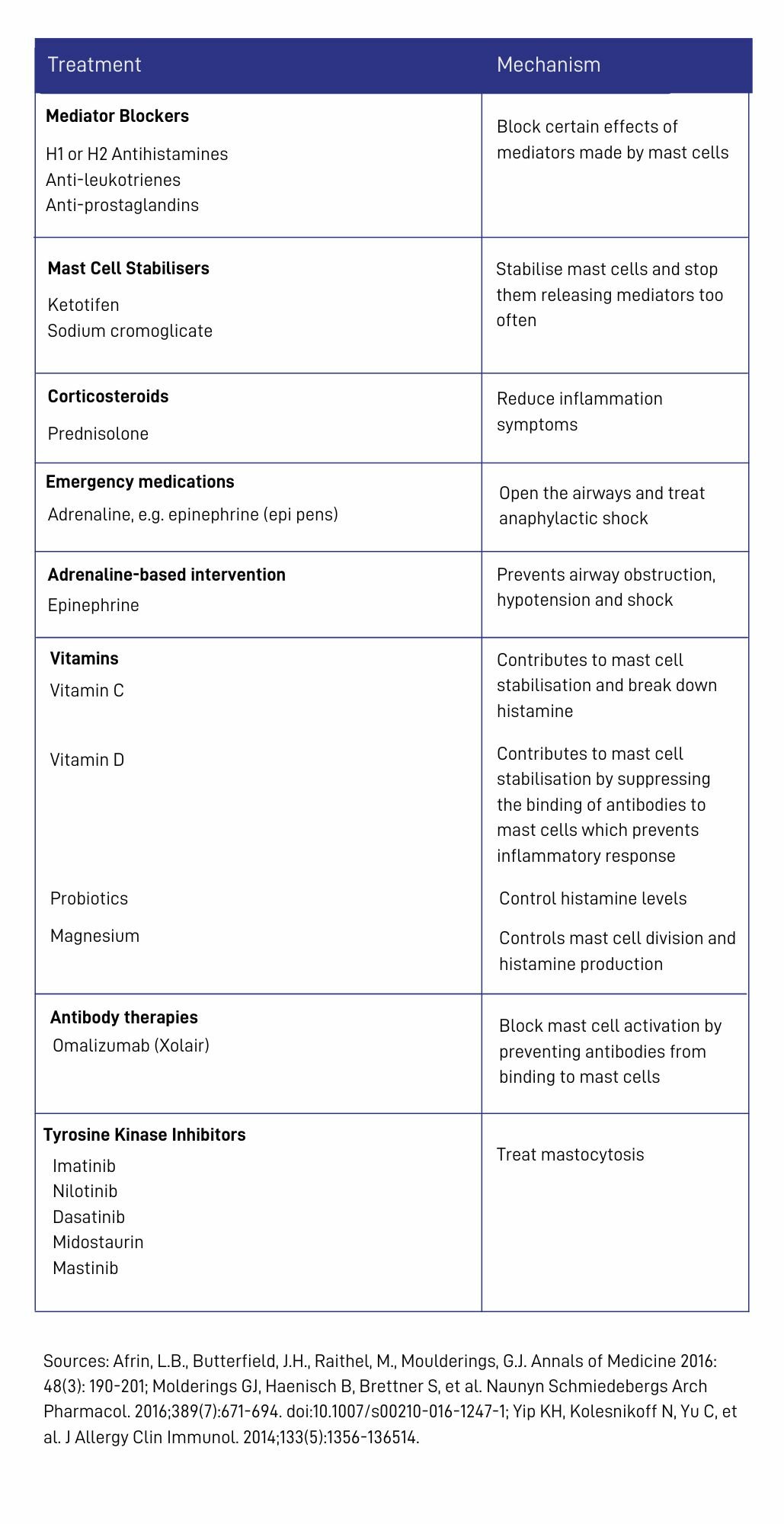
Medical Management
Various medications can be utilized to alleviate the symptoms of Mast Cell Activation Syndrome (MCAS). The table provides an overview of the medicines that have been shown to be effective for managing MCAS. The medicines are divided by whether they impact mast cell mediators or whether they help to stabilize or inhibit the mast cell itself.
Histamine blockers like H1 and H2s will mitigate the effects of histamine produced by the mast cells and are common recommendations as first-line defence if MCAS is suspected.
If you suspect you may be exhibiting clinical signs and symptoms associated with MCAS, we recommend reaching out to your primary care physician for more information. This can be a very challenging condition to identify in the context of Long COVID as its symptoms overlap heavily with other known conditions like ME/CFS and dysautonomia. Your doctor can discuss with you a trial of over the counter antihistamines to observe if there is any positive effect on your symptoms.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8459548/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10166245/#R21
- https://virologyj.biomedcentral.com/articles/10.1186/s12985-022-01891-2
- https://www.mastcellaction.org/about-mcas

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749