Call Us
updated Mar 29, 2021
by Courtney Steele
Registered Orthopaedic Physiotherapist
Back pain is one of the most common complaints we see at our clinics, because it’s just so pervasive. Between 50-75% of us will suffer from back pain at some point in our lives. The lumbar disc is a common source of back pain, so with that in mind I wanted to take a closer look at the issues surrounding lumbar disc pain: bulges & herniations.
A disc is a structure that sits between your vertebrae and acts as a shock absorber for your spine. Discs run up your whole spinal column in between each vertebrae from your back to your neck. 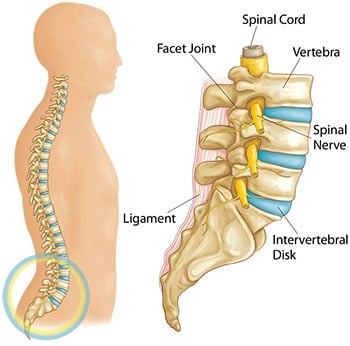
Disk bulge vs. Herniated disc
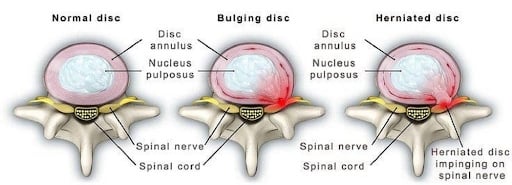
Even beyond bulges and herniations, there are many terms used to describe disc injuries, which can be confusing for patients (protrusions, extrusions, and sequestrations, for example). But there’s a reason for this! The different terms are used to describe the extent of the displacement of the nucleus and if there is a tear in the annulus or not. Now, sometimes these terms get thrown around interchangeably, but using the correct terminology is important as it directly relates to a patient’s symptoms, prognosis and it guides treatment.
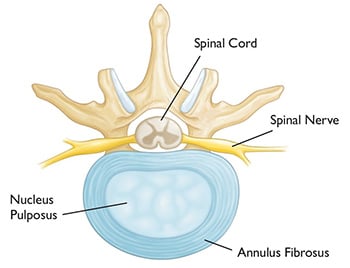
The main distinction that is important is if you are “bulging” or if your disc is truly “herniated”. A bulging disc describes a situation when the inner jelly is still maintained within the annulus fibrosis but it’s sitting in an area it shouldn’t be, which is usually a source of pain and discomfort. Disc bulges can be managed with conservative care like physiotherapy and this should be the first line of treatment.
If the disc is truly herniated though, that’s when the nucleus has broken through the annulus and has leaked into the spinal canal. This type of situation is less responsive to conservative care and recovery times in these situations are significantly longer compared to bulging discs.
One analogy that sometimes helps patients visualize these types of lower back injuries is the idea of a squeezed water balloon. If you squeeze the water balloon enough to deform it and stretch it, that’s akin to a disc bulge! If you squeeze the balloon so hard that it breaks and water spills everywhere, you’d be wet, and that would be a way of visualizing a disc herniation.
What causes a lumbar disc herniation?
As mentioned earlier, these types of situations are common, and disc bulges are the types of lumbar disc issues we deal with more than any other. Often, bulges are the result of gradual wear and tear – many patients report being fine and then bending over to pick up something innocuous like a pencil from their desk when they suddenly experience back pain. Bending over to pick up a pencil does not cause a disc bulge in a healthy back. But if there was underlying degenerative wear and tear it might have been enough to encourage the nucleus to move out of position.
Now, what causes degenerative wear and tear? It’s everyday movements that place stress on the discs in our back. Flexion (bending through your back) and rotation (twisting) – are the most stressful, especially when combined.
I know what you’re thinking: How can I go through life without bending over or twisting? Well, neither of these movements are dangerous or harmful in isolation (i.e. doing yoga or bending over to tie shoe laces), but they become harmful when we hold these non-neutral positions for long periods of time. So, slouching in an office chair, day-after-day, year-after-year, creates degenerative wear and tear on our discs, especially if we aren’t moving our backs in all the other ways it can and should move.
A true disc herniation is less common than a bulge but the mechanisms for how they develop are the same. One key difference is that herniations are more likely to occur from a traumatic event, like a car accident or a fall from height, or occur after years of episodic back pain.
Did you enjoy the water balloon analogy? Want another conceptual visualization? Think of your discs like jelly doughnuts! A jelly doughnut is enclosed but it is very responsive to pressure and movement! If you were to push on one side of it, it’s very likely the jelly is coming out the other side! This is what happens with herniations: If you place asymmetrical loads on these discs (i.e. pushing one one side of the doughnut), either over time or with excessive force, the nucleus (jelly) breaks through the fibres of the annulus (the doughnut).
What is a lumbar disc herniation with radiculopathy?
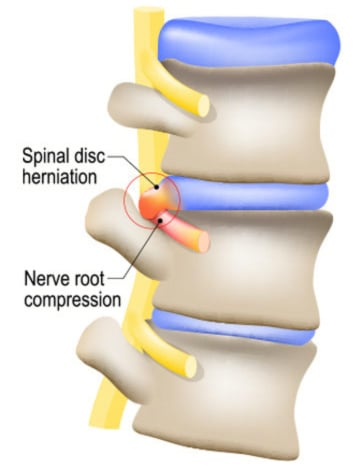
Disc bulges or herniations can result in what is called a radiculopathy (commonly described as sciatica). A radiculopathy occurs when the disc bulge is large enough to compress on the nerve roots that sit behind the disc. Often this is referred to as a ‘pinched nerve’.
These nerve roots carry the sensation and signal to generate strength in the muscles they supply. If you are suffering from radiculopathy, you will often experience severe leg pain or lack of sensation (numbness or tingling), muscle weakness and altered reflexes. To learn more about radiculopathy or sciatica, my colleague, and Advanced Practice (Spine) Clinician, Adam Brown wrote about it extensively here: https://cornerstonephysio.com/resources/what-is-sciatica/
How long do these disc herniations take to heal?
Most disc bulges resolve in 6-8 weeks, but it can take longer depending on the size of the bulge (i.e. if the bulge is hitting the nerve behind it like described above). One general rule of thumb: if you have leg pain associated with your back pain, that will extend the recovery timeline, and the further down your leg the pain goes, the further that extended timeline will go along with it. Meanwhile, if the disc is herniated, recovery time is likely in the six months to a year range if a non-surgical approach is being taken.
Can disc herniations heal on their own?
Both disc bulges and herniations will eventually heal on their own, but the how and why differ significantly. A disc bulge can heal relatively quickly (especially if it is your first episode of back pain). Even significant bulges do really well with conservative care (an individualized treatment plan from your physiotherapist will get you better faster). The typical treatment for this includes specific exercises where pressure is used to restore normal mobility to the spine. Depending on the size and direction of the disc bulge, a physiotherapist can guide you on which activities are safe, and which should be avoided!
If you have a herniation, it will heal on its own but some opt for surgery as it is a faster fix than the “wait it out” method, as these patients are usually in a lot of pain. Patients suffering from herniations can either wait for their body to naturally dehydrate this jelly-like material, or they choose a surgical path. Treatment options for herniated discs are more focused on pain management, maintaining mobility and strength, eliminating habits that are worsening the problem, and preventing atrophy that comes from disuse.
Meanwhile, if a patient is suffering from radiculopathy, some physiotherapists can provide acupuncture in the early stages for pain management when activity tolerance is low due to pain.
Speaking of pain management, it’s important to note that while doctors will often prescribe pain medication for these types of injuries, this helpful step does not treat the herniation or bulge directly!
Physiotherapy will help your back pain
No matter what path you’re on–disc bulge, herniation, or radiculopathy; surgical care or not–a physiotherapist will be able to do a detailed physical exam and guide you. They will help manage your pain, minimize your recovery time, and maximize your quality of life following your recovery.
If you are suffering with back pain, reach out for help! Book an assessment with a physiotherapist to get expert, individualized advice about your condition. We’re here to help!

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749