Call Us
updated Feb 16, 2021
by Courtney Steele MScPT
Pelvic Physiotherapist
Pelvic organ prolapse which is most commonly termed just “prolapse” is a condition in which there is descent/drop of the internal pelvic organs into the vaginal canal or completely out of the vagina or anus. Prolapse is the general term used to describe this descent but there are more specific medical terms used to describe what is actually prolapsing that you will likely hear if diagnosed with this by a medical practitioner.
Pelvic organ prolapse is a condition we treat often in our clinics. It effects approximately 40% of women between the ages of 50 and 79 years (1) and as the elderly and obese populations continue to increase, the incidence of prolapse is also expected to increase. Pelvic floor disorders as a result of prolapse can manifest in various ways, including urinary and defecatory dysfunction and physical discomfort. The constellation of issues that arise from pelvic floor disorders can cause psychological distress that leads to poor quality of life (1).
Although this sounds overwhelming, there is help! Prolapse is very successfully managed by conservative treatment and as we learn more about the risk factors and causes of prolapse we can improve prevention of developing this in the first place. Let’s take a look at the details – what is prolapse, what causes it and how can you treat/prevent it.
Types of Pelvic Organ Prolapse
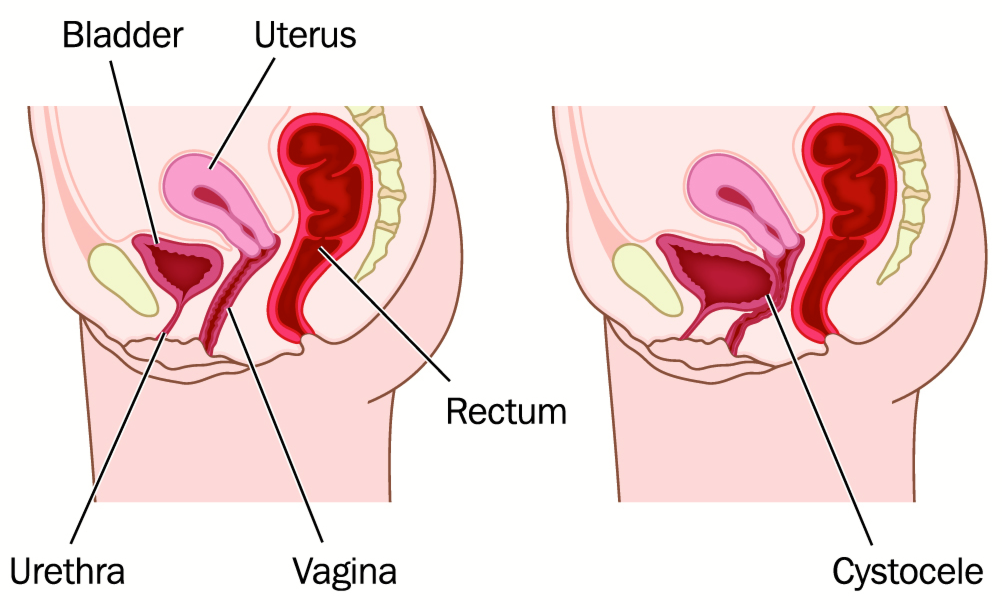
Cystocele (bladder prolapse)
The bladder sits on the front/anterior wall of the vagina so when this is prolapsing it is falling backwards into the vaginal canal
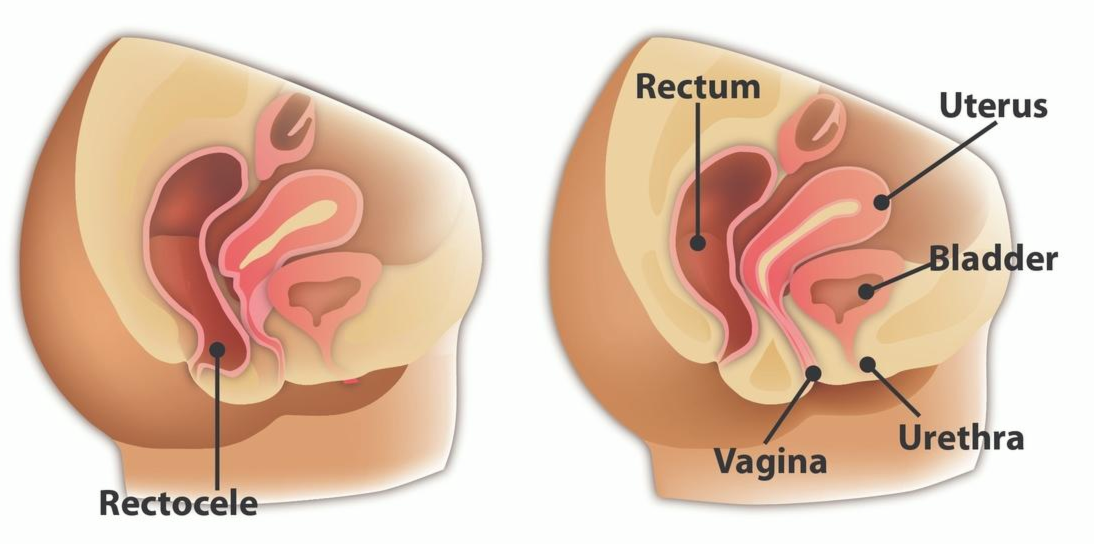
Rectocele
The rectum sits on the back/posterior wall of the vagina so when it is prolapsing it falls forward into the vaginal canal
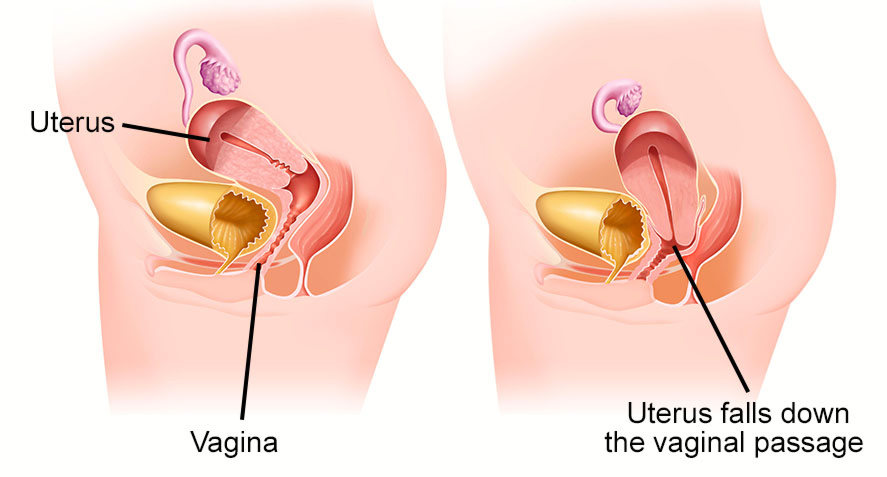
Uterine Prolapse
The cervix/uterus sits at the top of the vaginal canal and can drop down into the canal
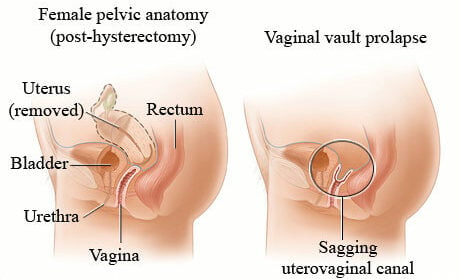
Vault prolapse
When you have had a hysterectomy (removal of the uterus) and the top part of the vagina descends down into the vagina
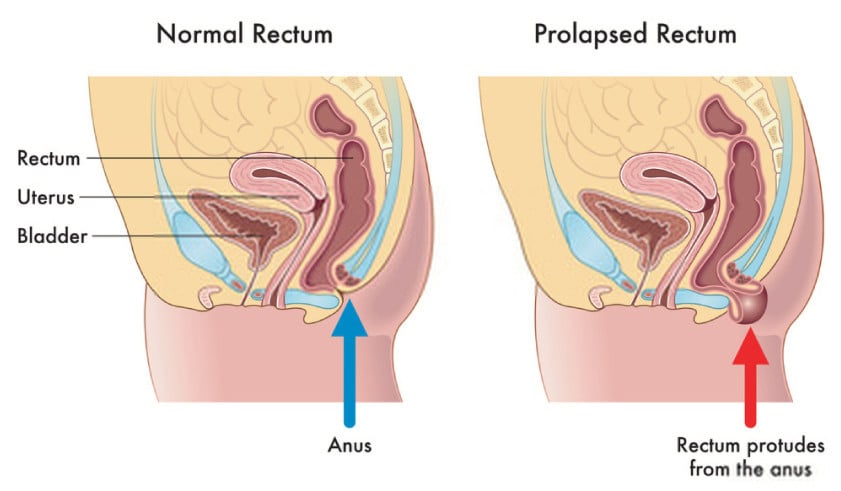
Rectal prolapse
This is when the rectum is being pushed out the anus vs. falling into the vaginal canal like a rectocele. Males or females can suffer with this.
How do you know if you have prolapse?
Prolapse is not generally a painful condition, the main symptoms include:
- A feeling of a bulge in the vagina (either physically when wiping, showering or a feeling of the descent with loaded activities such as walking or running)
- Heaviness of the pelvic floor of vulvar area – this is usually worse at the end of the day, or with impact activities that create more downward pressure (e.g. time on feet, lifting, running etc.)
Depending on the type of prolapse you are experiencing you can have other symptoms. These are more common with higher grades/significant prolapses
- Urinary retention (with a bladder prolapse/cystocele) – the feeling of incomplete emptying, the need to go to the washroom again shortly after having just emptied, increased frequency of urination. This happens as the bladder falls backwards into the vaginal canal so it is not sitting as upright as it normally would meaning the urine can’t drain as effectively into the urethra (think kink in a hose)
- Incomplete emptying during a bowel movement – this can occur with a rectocele for the same reasons above – the rectum isn’t as upright as it is normally so stool can “pocket” in areas leaving you with a pressure feeling that you didn’t fully empty
If you are experiencing any of the above symptoms you should see a medical practitioner to determine if these symptoms are indeed coming from a prolapse.
How is a prolapse diagnosed?
Prolapse can be diagnosed on a routine vaginal exam by any trained provider (i.e. your family doctor, OBGYN or pelvic physiotherapist). During the exam they will generally get you to bear down (create downward pressure) and watch for descent of the pelvic organs. This mimics what is happening when you stand and gravity and your body weight is acting on these organs. Prolapse is graded (0-4) by the amount of descent (how far it drops into the vaginal canal) and termed by what organ is prolapsing.
The grade of prolapse has to be taken into account with the amount of symptoms the person experiences. Many women (40-50%) will have a mild prolapse but these are often asymptomatic – there are no major health concerns of a mild asymptomatic prolapse.
When determining treatment options it is more important to listen to the symptoms and how significantly the prolapse is affecting a person’s life than to base it on grade alone. In part, this is because the grade of prolapse can change day to day, depending on time of day and what has been happening recently in the patient’s life. For example if you have been doing a lot of heavy lifting lately you might have a higher grade/more symptoms of your prolapse at this time then during a regular week.
How often and with what activities you have symptoms gives a better picture on how you are managing the pressure systems in your day to day life vs. a moment in time during the exam.
What are the risk factors for developing prolapse?
Your pelvic organs are held up by ligaments/endopelvic fascia and your pelvic floor muscles. So anything that puts downward pressure/strain on your ligaments/fascia or pelvic floor muscles increases the risk of prolapse.
Risk factors for prolapse include:
- Pregnancy and previous vaginal deliveries (risk increases with multiple births) – think of the pressure of carrying a baby to term and then the pressure created by pushing during delivery – the type of delivery, if assisted delivery techniques were used and length of second stage can all be factors
- Chronic constipation (think mini-childbirth)
- Excess weight (especially excess weight in the abdomen)
- Regular valsalva maneuvers (holding your breath when doing a difficult task i.e. lifting something heavy). It is much better for your pelvic organs and muscles to dissipate some of this pressure by exhaling when you lift
- Smoking (this weakens all tissues)
- Menopause (due to lower Estrogen causing thinning of tissues)
- Age
- Genetics
- Weak pelvic floor
How is Prolapse treated?
Prolapse is generally very well managed with conservative care. “Pelvic floor muscle training is effective and cost-effective in reducing prolapse symptoms and should be recommended as first line management for prolapse” (2)
Physiotherapy for prolapse
Your pelvic physiotherapist will do a detailed assessment to determine the extent of your prolapse and what factors you need to address to improve it. This will most often involve:
1) Assessment and Exercise Prescription
An assessment of your pelvic floor and core strength/endurance and teaching you exercises (kegels and other core exercises) to improve this. These exercises are individualized depending on your initial strength, endurance and activity goals. Many women don’t perform kegels properly so it is worth having this assessed to ensure you are doing this effectively. Research shows that pelvic floor muscle training leads to a reduction of prolapse symptoms (3).
2) Lifestyle Modifications
This again will be individualized depending on your symptoms and goals but often will include:
Activity recommendations (what is safe given your current state) and a progressive program to get you back to doing what you love symptom free
Education on how to mitigate other risk factors such as:
– Constipation (fiber diaries and education)
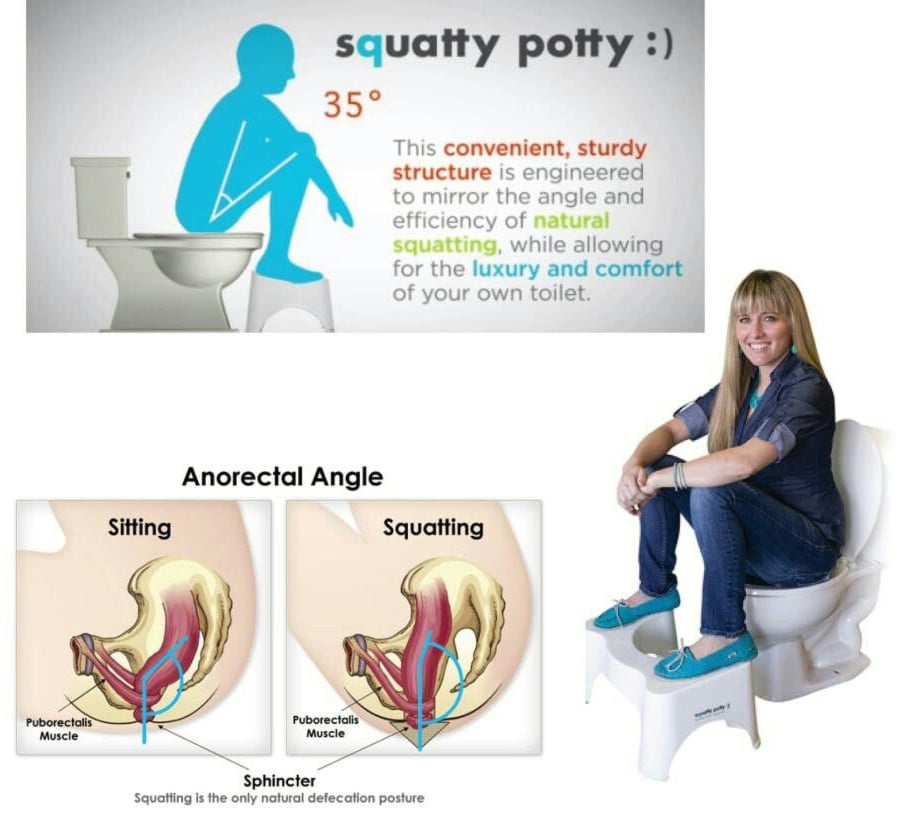
– Toileting mechanics that help reduce straining (i.e. feet elevated on a stool like the squatty potty as well as proper breathing and pushing mechanics)
– Proper lifting strategies and breathing mechanics around this to dissipate pressure on your pelvic floor
– Importance of proper posture and sitting habits
3. Device Recommendations
Recommendations on tools or factors to help manage symptoms associated with the prolapse
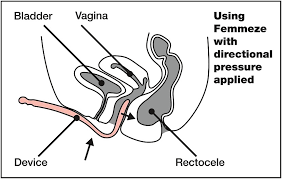
The femmeze tool or other similar tools for incomplete emptying of your bowels with a rectocele to avoid pocketing
Toileting mechanics and strategies to help with incomplete emptying of the bladder with a bladder prolapse.
4. Prevention
Birth preparation – seeing a pelvic floor phsyio prior to delivery can help you to learn proper pushing techniques, best positions to labour in to allow you to birth in the most effective and least strenuous way to your pelvic floor – see our blog on how to prep for childbirth for more information on this.
Education about other treatment options depending on the activities you want to get back to to allow you to do so with less strain on the system and progression of the prolapse (i.e. pessaries)
A general check of your pelvic floor strength and endurance is recommended so you know if you should be working (and how) on these muscles to improve the support of these organs (especially postpartum and as you age)
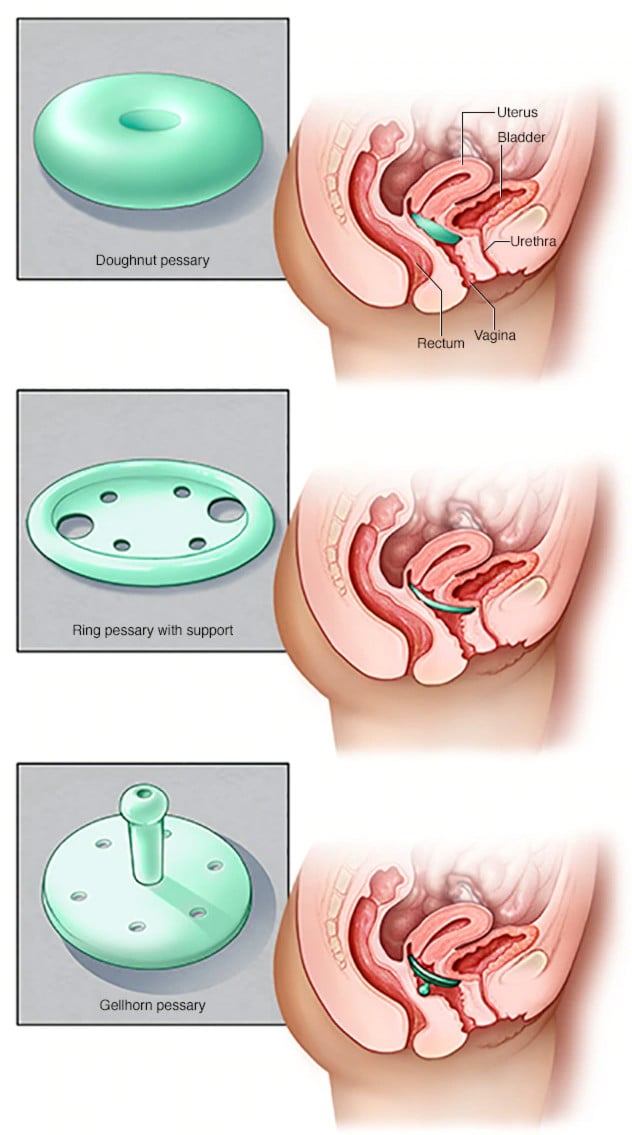
Pessaries
A pessary is a device that is inserted into the vagina (much like a tampon) to support the prolapse and prevent further strain on the ligamentous system. There are many different shapes, sizes and considerations that need to be accounted for when determining which pessary is right for you.
These are fitted by a medical professional that has training in this to ensure you have one that is comfortable, is the right size/shape and fits your lifestyle needs.
If you aren’t sure if you want to commit to a pessary or have a mild prolapse there is an off the shelf product we often will recommend for patients – Poise Impressa. Although this is marketed as an incontinence device due to its shape and materials, it acts very much like a pessary. This works best for mild prolapses. I often recommend this to patients if they want to continue with higher impact activities to prevent progression of the prolapse/strain on the ligaments and fascia. It looks very much like a tampon and you can wear it for up to 8 hours or just insert it in for higher impact activities and remove afterwards.
Vaginal Estrogen
This may be recommended by your doctor if you are suffering with prolapse after menopause. Estrogen creams or tablets can be used to improve the vaginal strength and health of tissues.
Surgery
Surgery can be helpful in treating the symptoms of prolapse; however it is important to consider this is a significant surgery and the success of conservative measures (pelvic floor strengthening and/or pessary) is very strong with less side effects. Generally speaking (as long as you have a grade 3 or less) it is recommended you try pelvic floor strengthening (under the guidance of a pelvic physiotherapist) for 3 months and a trial of a pessary before considering surgery.
Depending on the extent and what is prolapsing the type of surgery varies – some are done vaginally and others laparoscopically. To determine if surgery is the right option for you it is best to speak to an OBGYN who specializes in these surgeries. It is important to note that if you do choose surgery as your management option once cleared by your surgeon you should consider seeing a pelvic floor physiotherapist to work on strengthening the pelvic floor as this can improve postoperative outcomes.
What exercises are safe/can I do with pelvic organ prolapse?
Choosing the right exercises for you is important to improve and prevent symptoms. What the right exercises are for you will be different for someone else as it depends on overall strength, endurance and severity of prolapse. A good general rule of thumb is if an activity is causing symptoms (i.e. a feeling of heaviness or a bulge) then you shouldn’t be doing it at that stage. This is not to say never do this activity again but you will need to improve strategies/strength before you can perform it symptom free or use a supportive device like a pessary during it.
Generally speaking low impact exercises are more tolerated by prolapse patients as they minimize stress on the pelvic floor (i.e. swimming, biking, water aerobics, low impact aerobics, walking). Higher impact exercises such as running, jumping and heavy lifting place more strain on your pelvic floor so are less tolerated – but can be worked towards if these are your goals.
Working with a pelvic floor physiotherapist will help you determine what is best for you to start with and work safely back to the activities you love to do. Cornerstone Physiotherapy provides skilled pelvic physiotherapy in Toronto, North York and Burlington. Contact us today … we are here to help!
References
- Conway C, et al. Pelvic Organ Prolapse: A Review of In Vitro Testing of Pelvic Support Mechanisms. Ochsner Journal. 2020
- Hagan S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011 Dec 7;(12).
- Hagen S, et al, Pelvic floor muscle training for secondary prevention of pelvic organ prolapse: a multicentre randomised controlled trial. www.thelancet.com Jan 28 2017.

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749