Call Us
by Rosie Mahendran
updated July 15, 2020
There are many ways we can prepare for the birth of a child, from prepping your home to learning about nutrition – the topics are endless. In this discussion, I want to highlight the best practice to prepare for the labour and delivery of your baby. I understand that sometimes we take the “we’ll just figure it out attitude” (which you will!), but remember knowledge can be powerful.
BEFORE LABOUR AND DELIVERY
1. Choose your health care team, providers and setting.
Should I see an OBGYN or a midwife?
The best answer here is whoever you feel the most comfortable with. Some practical things to know is that the OBGYN who takes care of you during your pregnancy may not be the doctor who delivers your baby. Alternatively, the midwife will typically follow you during birth, delivery and 6 weeks postpartum. They have different training, as midwives are trained in low risk pregnancies while OBGYN’s are both low and high risk. Please refer to this article to help you with more information: https://www.theglobeandmail.com/life/health-and-fitness/ask-a-health-expert/midwife-family-doctor-or-obstetrician-who-should-handle-my-prenatal-care/article13857840/
Who should be a part of my birth team?
The research shows that continuous presence of an individual who provides emotional support, comfort measures, advocacy, information and advice during labour helps assist with improved outcomes. These outcomes include, increased likelihood of a vaginal delivery, decreased the use of epidurals, improved APGAR scores and maternal satisfaction. These individuals can include a trained person such as a doula, midwife, nurse and/or friend/family member (SOGC Clinical Practice Guidelines, 2018).
How can pelvic floor physiotherapy help during pregnancy?
Prenatally, pelvic floor physiotherapy is used as a preventative measure and a way to prepare physically and mentally for labour and delivery. This type of therapy can assess the individual and provide information on:
- how to perform Kegels
- how to relax the pelvic floor muscles
- what exercises to partake in
- how to push effectively during labour
- what birthing positions are optimal for labour
- how to perform perineal massage
- how to perform mindfulness/breathing strategies during labour/contractions
- what to expect postnatal
- how to help with low back and pelvic girdle pain
There is strong evidence that pelvic floor muscle training (PFMT) with a physiotherapist is recommended to prevent urinary incontinence during pregnancy and after delivery and core training is recommended to prevent and treat low back and pelvic pain during and following pregnancy (Hay-Smith et al 2008, Joint SOGC/CPA Policy Statement, 2005)) .
Can massage help during pregnancy?
Prenatal massage can help women decrease tension, decrease pain and increase relaxation which promotes overall positive effects for the birthing experience. Prenatal massages can be effective but if you do not have access to massage, gentle touch or pressure from a loved one works as an alternative.
2. Attend a prenatal class.
A prenatal class can cover a wide array of topics and although it is important to attend a prenatal class I also recommend looking into classes that help teach relaxation strategies to prepare your physically and emotionally for birth. An example of this is hypnobirthing. Often these classes are great when paired with pelvic floor physiotherapy as it can help increase awareness to the pelvis and reduce potential fear and anxiety around the delivery.
3. Make a birth plan!
A general outline of how you want your birth to go can be a great idea. Remember this plan can be modified as you learn more and may not always go accordingly so stay flexible! Your birth plan can include:
- How you want to deliver and where (ex, 4 point kneeling and at a birthing center)
- If you want medical interventions and which ones
- How you want to manage pain
- Who you would like in the delivery room
- How you would like to spend the stages of labour (ex. 1st stage in standing)
4. What types of exercises are safe for me to do during pregnancy?
Exercise is shown to reduce the risk of common complications due to pregnancy. Most exercises have been deemed safe for women according to the Canadian Guidelines for Physical Activity during Pregnancy unless you have contraindications (communicated to you by your healthcare provider). What a better question would be is what exercises are not safe for me during pregnancy? Women should be cautious about activities that involve physical contact or may involve falling, activities at high altitudes and activities performed in high heat. These activities may include: hockey, horseback riding, gymnastics, Olympic lifting, hot yoga, skiing. Otherwise, the recommendations are that pregnant women should:
- Accumulate 150 mins/week of moderate physical activity to reduce complications within pregnancy
- Accumulated over a minimum of 3 days with everyday strongly recommended
- Incorporate aerobic and resistance training exercises as well as yoga/gentle stretching for added benefits
- Pelvic floor muscle training (if deemed appropriate by your physiotherapist)
- Maintain adequate nutrition/hydration – drink water before, during and after physical activity
If you were previously inactive you are still encouraged to start physical activity in pregnancy. You may need to begin slower, at a lower intensity and progress gradually. It’s highly recommended you consult a physiotherapist or a fitness professional that works with pregnant individuals to help you progress these activities safely.
5. How do I manage my pregnancy during the COVID-19 era?
Staying at home and physical distancing is the best practice to keep you and your baby safe. This might include switching your in-person medical appointments to telehealth. Please visit https://www.canada.ca/en/public-health/services/publications/diseases-conditions/pregnancy-advise-mothers.html for more information regarding best practices during this time.
DURING LABOUR AND DELIVERY
1. When should I go into the hospital/birthing centre?
If possible try to spend as much of your labour at home. It is believed that your home can help maintain comfort and as well prevent the use of medical interventions earlier than needed. Typically, you will not be admitted into the hospital until you are 4cm dilated so you can use the 4-1-1 or 5-1-1 rule to estimate what is an appropriate time to go to the hospital or call your midwife. This is when the contractions come every 4 minutes, they last 1 minute in duration and this has been happening for an hour.
2. How do I manage my pain?
Many individuals will elect for an epidural to help with any pain experience. If you choose to get an epidural the newest guidelines state that it can be done whenever you need it and based on your choice (SOGC, 2018) . It is important to remember that the epidural requires you to stay still for a certain period of time, so if you are unable to due to pain the anesthesiologist cannot safely administer it.
Other ways that have helped a positive birthing experience and pain include reducing stress. Stress can ramp up your pain experience and also dampen the good hormones we need to facilitate the birthing process. We can reduce stress and pain by:
- creating a calm, environment – this can be achieved by music, low lighting and emotional support
- perform breathing exercises, relaxation/mindfulness techniques, gentle exercises/stretches
- Transcutaneous electrical nerve stimulation (TENS)
- Acupressure/acupuncture
- Heat/cold therapy
- Massage/gentle touch
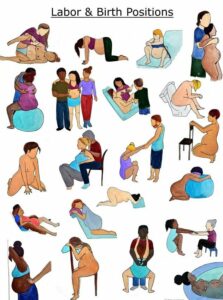
3. What is the best position to deliver my baby?
Women are often on their backs in hospital however, there many benefits to upright positioning. When laying on your back you increase the pressure to the back of your pelvis and we want to disperse pressure to the vaginal opening. This can help decrease the use of instrumentation and episiotomies.
A general rule is to assume the most comfortable position for you. You may want to try out these different positions with your health care provider to see which one feels the best for you. Some positions can include:
- 4 point (hands and knees)
- Side lying
- Squatting between partners knees
- Seated on birth chair
- Kneeling
- Knees to chest
Note that if you receive the epidural you will be limited to positions such as laying on your back or in side-lying.
4. How do I push?
Often times the Valsalva manoeuvre is used to push (forced exhalation on a closed airway) however, research shows we should limit this manoeuvre in pushing and try an open airway technique instead. Such techniques can include: low sounds, humming, pursed lip breathing. These techniques can relax the muscles and facilitate softening of the muscles to help assist in delivery.
AFTER LABOUR AND DELIVERY
1. What do I need to do after birth?
For the first 3 days think about rest, ice, compress and elevation (RICE principles) to help with managing the pain and swelling. Rest (as much as possible under the circumstances) will also help with decreasing your cortisol levels which will improve your healing. We want to avoid excessive force on the healing tissue which may include managing any potential constipation or using some tools to help with easing bowel movements. You can also start gentle pelvic floor muscle training that is pain free – this can help reduce the swelling and feelings of pressure. In this period if you are feeling overwhelmed or have any negative emotions it is important to seek the appropriate care such as maternal support groups, doula, psychologist, etc. Remember you are not alone!
Whether you had a vaginal delivery or cesarean section, at the 6 week mark you should have a check up with your OBGYN/midwife, who will assess the integrity of the tissues. They will deem you safe to return to activities however, they are basing this on tissue healing and not the symptoms you are experiencing. In France, postnatal women are encouraged to attend 6 pelvic floor physiotherapy sessions (covered by the government) to prevent or treat pelvic floor dysfunctions. Symptoms can present later in life so starting early will help set you on the right track. Postnatally, pelvic floor physiotherapists will assess are:
- Pelvic floor muscles (strength/length)
- Integrity of C-section scar or vaginal tears
- Your thoughts/beliefs/attitudes and how it affects your physical well-being
- Rectus diastasis (separation of the abdominal musculature)
- Readiness to return to activities
2. When and how can I return to activity or play?
When your physician/midwife has assessed you stitches/scar they will deem you safe to return to activities. You can start with gentle activities (reduced intensity and length) such as yoga, gentle pelvic floor exercises, mommy and me fitness class. You want to monitor for symptoms (such as pressure/heaviness vaginally, incontinence, pain) and if you experience any symptoms scale back the activity or stop. Working with a pelvic floor physiotherapist can be helpful to ease back into activities safely as there are no specific guidelines for exercise for postpartum women.
If you have any questions on how to manage your pregnancy or prepare for childbirth we recommend you set up an appointment with one of our pelvic floor physiotherapists. These appointments can be conducted virtually to accommodate physical distancing. Furthermore, you may opt to use our complimentary 10 minute phone consult with a Registered Physiotherapist for more information!
Rosie Mahendran MScPT
Pelvic Health Physiotherapist
Rosalina is a highly experienced physiotherapist with specific credentials in managing pelvic health conditions. She has a particular interest in pregnancy related dysfunctions and consistently achieves excellent outcomes with her patients. Rosie practices at Cornerstone’s downtown pelvic health clinic.

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749