Call Us
updated June 2, 2021
by Courtney Steele MScPT
Pelvic Physiotherapist
Endometriosis is a condition in which tissue similar to that which lines the inside of your uterus (endometrium) grows outside of your uterus. This growth occurs in the abdominopelvic cavity and thus commonly affects pelvic organs like the bladder, ovaries, bowel and pelvic ligaments.
What are the symptoms of Endometriosis?
Endometriosis usually begins as intense period pain. Every woman has experienced some type of discomfort and cramping during periods, but this pain is different! It causes women to take time off from work or school, or to stop participating in physical or social activities. Typically this significant cyclical pain turns into persistent pain.
Common symptoms include:
- Painful periods
- Heavy bleeding during menstruation
- Painful Intercourse
- Fatigue
- Bloating
- Bowel Changes during menstruation (i.e. become constipated and find it difficult to pass stool during this time)
- Nausea
- Fertility Challenges
What does Endometriosis pain feel like?
The pain associated with endometriosis typically occurs all around the abdominopelvic cavity. Most women will have lower back pain, abdominal pain and pelvic pain (vulvar pain, pain deep inside the pelvis with anything inserted into the vagina – tampons, menstrual cups, during sex etc).
Endometriosis and fertility
According to The Society of Obstetricians and Gynaecologists of Canada, endometriosis is found up to five times higher in those people who struggle with infertility, compared to the general population. The link between endometriosis and infertility is not fully understood at this point, as some with severe endometriosis have no fertility issues, while others with a very low stage, have fertility struggles. One thought is that the link might have to do with scarring from lesions or surgeries around the ovaries, uterus and fallopian tubes.
How is Endometriosis diagnosed?
For a variety of reasons, diagnosing endometriosis can be challenging. While most people with endometriosis do present with some symptoms, most also have normal physical gynecologic exams (think PAP test) (2). However, these exams are often painful for those with endometriosis, because of tension in the pelvic floor muscles, and sensitivity deeper in the vaginal canal.
To fully confirm an endometriosis diagnosis, you need to either undergo a laparoscopic inspection/biopsy or a transvaginal ultrasound (a transabdominal ultrasound will not be able to detect endometriosis).
If you are suffering with significant pain during your periods please talk to a medical professional and ask them if it might be a possibility you have endometriosis. If endometriosis is confirmed, it can drastically change your treatment options, and knowing the severity of the issue and what organs are affected allows you to have a more informed, personalized discussion with your surgeon about options moving forward.
According to EndoAct Canada, 1 in 10 women will have endometriosis in their lifetime; more than one million Canadians currently suffer with endometriosis; and on average, Canadians wait five years for a diagnosis, and nearly two years more for surgery.
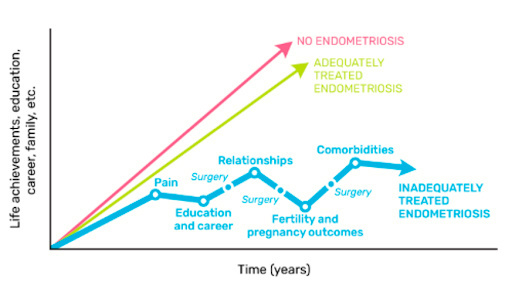 * image courtesy of EndoAct Canada
* image courtesy of EndoAct Canada
Diagnosing Endometriosis with transvaginal ultrasound
A transvaginal ultrasound needs to be performed by a specialized practitioner trained in identifying endometriosis. There’s currently only one in the GTA at McMaster University (https://mathewleonardi.com/), but the hope is that more will become available in the near future.
Typical transvaginal ultrasounds are used to visualize the uterus and ovaries but when you see a practitioner who is specially trained to identify endometriosis, they can use the ultrasound to visualize other areas where endometriosis is more commonly found. This allows for a: non-surgical diagnosis, staging of disease and an informed discussion around surgical recommendations based on severity and organs affected.
For more info on diagnosing through transvaginal ultrasound, here is an interview with Dr. Leonardi from the McMaster University Endometriosis Clinic.
Diagnosing Endometriosis with biopsy/exploratory surgery
Right now, exploratory surgery is more commonly used than transvaginal ultrasound to diagnose endometriosis, mainly because it’s more accessible.
It is minimally invasive, using small incisions to insert a microscopic camera into the abdominopelvic cavity to visualize and biopsy the tissue.
What causes Endometriosis?
We don’t know much about what causes endometriosis. We know it usually develops several years after menstruation begins, and there is a hereditary link: You are at greater risk to develop endometriosis if one or more of your close relatives (mother, aunt, sister) has it.
How does Endometriosis cause pain?
Whether it’s pain from a paper cut, a headache, or endometriosis, all pain in our body is created and controlled by our central nervous system.
Our nervous system is in a constant state of communication, monitoring our body’s state and responses.
With persistent pain, our nervous system has been signaling about it for an extended period of time, and it can cause itself to become centrally sensitized. Essentially, it goes into high alert mode, creating a pain response for situations that, under normal circumstances, wouldn’t pass the threshold of a “threat” to the system. In these situations, even a light touch, or the feeling of clothing can be painful!
To exacerbate the situation, the nerves in close proximity to the “high alert” area try to help out, sending even more signals to the brain! So, the pain becomes more widespread. For example, pain that begins in your pelvic floor can spread to cause back, abdominal, and bladder pain.
So, essentially, when a nervous system is centrally sensitized, pain can occur in areas of the body that don’t have any actual physical problems, simply because the nervous system’s alarms are all going off.
This is the state nearly all of my endometriosis patients are in. So, understanding what’s going on in your body, and how to calm your nervous system (i.e. turning off those alarms) is essential to managing the pain of endometriosis over a long period of time.
How is Endometriosis Treated?
Treatment for endometriosis MUST come for a multidisciplinary team to achieve best results and management. While medical and/or surgical intervention in endometriosis may be effective, they are not a ‘magic bullet’ and do not stand alone (3).
Surgery is the only way to rid your body of endometrial implants but those implants are unlikely the ONLY source of your pain so you need to address all factors affecting pain in order to have the best results.
Your team may include: doctors (family MD, OBGYN, surgeons), pelvic health physiotherapist, psychotherapist, nutritionist and/or a naturopath.
Below are some examples of avenues of care/management you may want to explore.
1. Medications
Early in treatment, hormonal-based therapies are often used to reduce the pain associated with endometriosis. Reducing estrogen levels is often the goal of these medications. This is often attempted by using “the pill,” an IUD, or other hormone-related medications such as aspen-dienogest/visanne.
Suggested treatment cycles usually span two to three months. Some patients find this avenue very helpful in managing their symptoms, but it is important to note that this course of action does not eliminate your endometrial implants. It suppresses them and may slow their growth.
Other medications for pain relief are also commonly prescribed (commonly anti-inflammatory medications such as ibuprofen or naproxen).
Support for cannabis and CBD for medical management of persistent pain is also growing (3) although this should be discussed with your doctor to ensure you are using the appropriate combinations that best address your condition.
2. Pelvic Physiotherapy
A pelvic physiotherapist can help you to understand your pain, manage your symptoms and improve your quality of life.
“Pelvic physiotherapy is increasingly being recognized as an important component of the multidisciplinary treatment approach to endometriosis (5)(6), especially when there is coexisting chronic pelvic pain. The British Pain Society (2013) considers a physiotherapist an essential member of the multidisciplinary team for patients with chronic pain.” (7)
We, as pelvic physiotherapists, focus a lot on pain education and calming your sensitized nervous system in order to help you manage your overall pain levels more effectively.
Calming a sensitized nervous system is imperative before you undergo surgery because it has been shown to improve surgical outcomes. Patients I have seen who have had surgery when their system is highly sensitized do not do as well immediately post-op compared to those who have worked on calming their nervous system before the surgery.
And it’s important to note, it’s not because the surgery wasn’t successful in removing the endometriosis or that it wasn’t the right treatment option. But their body was still in a high-alarm state. This is why it is important to be working with a pelvic floor physiotherapist from the beginning of your healing journey. We will focus on pain education and different approaches to help calm your nervous system (i.e. breathing techniques, mindfulness and meditation, and gentle activity). This will help you to manage your pain more effectively and also will lead to better post-op outcomes if surgery is part of your treatment plan.
We also work directly with the pelvic floor muscles that are often in a protective guarding/spasm state. When your pelvic floor muscles are tight and unable to relax, it can lead to pain in all sorts of scenarios (vaginal penetration, back pain and difficulty/pain passing urine/stool).
And we also prioritize getting people back to physical activity. We can advise on which activities are well-tolerated and can help with pain; and can help with generalized re-conditioning and coaching.
Learn more about Cornerstone Physiotherapy’s Pelvic Health Clinic here.
3. Lifestyle Changes
There is a significant amount of literature supporting mindfulness, meditation, restorative yoga, qi gong, tai chi and other gentle calming types of inputs/exercises that help to manage persistent pain. Identifying a few of these activities that work for you and fit with your lifestyle can reduce your pain, and improve your overall quality of life.
4. Diet
Eating a healthy diet is important for many with endometriosis. Many people who suffer from endometriosis find certain foods exacerbate their symptoms. There is evidence starting to come out supporting the theory that an anti-inflammatory, low FODMAP or gluten free diet can help to manage symptoms. Also ensuring you get enough fluid and fibre is important to avoid constipation. Speak to a nutritionist or a naturopath to find help in this area.
5. Sleep
It is common to have sleep issues when you suffer with endometriosis. Generally, we should all be aiming for seven to nine hours of sleep a night. There isn’t much research on the management of sleep in women with endometriosis, but one randomized controlled trial (RCT) implemented an administration of 10 mg of daily melatonin, which was found to improve the quality of sleep, reduce pain scores and reduce analgesia use (4).
6. Counselling
Therapy can help to address the psychological aspects of persistent pain. Many people who suffer with persistent pain experience high levels of stress, anxiety, and depression. The fact that endometriosis is often linked to painful sex can greatly impact relationships, and many couples struggling with this benefit from talking to a sex therapist.
7. Surgery
Every surgery for endometriosis is different. It will depend on a multitude of factors including: your age, if you are still hoping to have children after your surgery, the extent of the endometrial implants and where they are located.
Whenever possible excision surgery (and not ablation) should be performed – this is the gold standard.
While both procedures are minimally invasive and are performed laparoscopically, ablation surgery burns off only the surface of the implants, whereas excision surgery gets at the whole implant.
A garden metaphor can help to understand the difference. Ablation is like picking a dandelion at the base of the stem – it is likely to grow back, while excision is like pulling a weed from the roots – unlikely to re-grow.
It’s important to note that sometimes a hysterectomy is suggested for those suffering from endometriosis and although this can be helpful, it does have other risks associated with it.
The whole patient picture needs to be taken into account when making the decision about what the best options are for that individual.
And always remember that despite surgery, people often still have pain because of central sensitization that has occurred from years of suffering, so getting rid of the endometriosis lesions via surgery is likely only part of a full solution.
Although there is no cure for endometriosis, there are a lot of treatments and ways you can manage your symptoms. It is a challenging condition, but by following all these steps, and with help, you can hopefully live the life you want and not be held back by your pain.
I hope you found this article helpful in understanding endometriosis and the options for management. I’ve included some links below that I’ve found to be great resources for my patients, and I sincerely hope they help you too!
RESOURCE LINKS:
Self management strategies for endometriosis. Human Reproduction Open, pp. 1–11, 2020 – Download Here.
EndoAct Canada
support group, patient only facebook groups, online monthly restorative yoga, QiGong, and cooking class.
Endometriosis foundation of America
lots of information on the site, including endo TV, endo news, international patient conference 2018 to 2021.
Beating Endo By Dr. Iris Kerin and Amy Stein (DPT)
Relaxation/breathing exercises: https://www.beyondblue.org.au/get-support/staying-well/relaxation-exercises
REFERENCES
1. Leonardi, M et al (2020). Ignored Because It Is Benign – It Is Time to Treat Endometriosis as if It Were Cancer. Journal of obstetrics and gynaecology Canada. doi:10.1016/j.jogc.2019.12.014
2. Parasar, P., Ozcan, P., & Terry, K. L. (2017). Endometriosis: Epidemiology, Diagnosis and Clinical Management. Current obstetrics and gynecology reports, 6(1), 34–41. doi:10.1007/s13669-017-0187-1
3. Leonardi, M et al (2020). Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic . Human Reproduction Open, pp. 1–11, 2020 doi:10.1093/hropen/hoaa028
4. Schwertner et al. 2013. Efficacy of melatonin in the treatment of endometriosis: a phase II, randomized, double-blind, placebo-controlled trial. Pain, 54(6):874-81. doi: 10.1016/j.pain.2013.02.025.
5. Ball and Khan, 2020 Recent advances in understanding and managing chronic pelvic pain in women with special consideration to endometriosis. F1000Res. 2020; 9.
6. Findeklee et al., 2020. Treatment algorithm for women with endometriosis in a certified Endometriosis Unit. 2020 Feb; 72(1):43-49.
7. The British Pain Society. Guidelines for Pain Management Programmes for Adults. 2013, London: The British Pain Society. [Google Scholar]

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749


