Call Us
updated Feb 14, 2021
by Joon Nah
Certified Vestibular and Concussion Physiotherapist
What is Post Concussion Syndrome?
A concussion is a change in normal brain functioning as a result of exposure to a mechanical force. It is often called an mTBI (minor traumatic brain injury) and can involve direct or indirect head impact.
It can be more specifically defined by any of the following:
- any period of loss of consciousness
- loss of memory before or after the incident
- an alteration in mental state at time of the injury
- a focal (or specific) neurological issue following the incident
Concussion vs Post Concussion Syndrome
Post concussion syndrome is where the symptoms related to a concussion have persisted past the initial 7-10 day period of time. Concussions that are more severe, or have several symptoms, are more likely to transition to post concussion syndrome, as can a lack of proper management of an initial concussion. In fact, one study showed that up to 84% of concussions end up with this chronic diagnosis of post-concussion syndrome or PCS (1).
This figure adds up when you consider that nearly 300,000 traumatic head injuries are reported yearly in Canada (2). And almost half of the population has experienced a concussion in their lifetime (3).
What happens with a concussion?
Your brain is surrounded by layers of soft tissue (meninges) and cerebrospinal fluid. This acts like an insulating cushion for your brain by allowing it to gently move within the skull as you move your head and body.
A concussion involves a sudden deceleration or stop in head movement. Examples include: striking your head on the floor after falling down the stairs; a football player being struck by an opposing player as they are moving forward; a driver’s head snapping from side-to-side as she is “T-boned” by another car. This rapid forceful stop creates excessive movement of your brain inside your skull (too much than the surrounding “cushion” can protect against). This results in the initial cause of damage to brain tissue, nerve pathways, and neural cells that occurs with a concussion.
A concussion does not have to involve a direct impact, such as your head hitting the ground. Often quick acceleration/deceleration motions where the head doesn’t strike anything, (such as with whiplash) can cause more significant injuries.
A concussion causes the following injuries to the brain:
1) Direct “bruising” to areas of the brain that strike the walls of the skull as it moves or “bounces” within it.
2) Tearing, shearing and stretch injuries to nerves and small blood vessels. This usually affects deeper areas of the brain and regions close to the brain stem.
3) A change in the brain’s chemical balance, which has a toxic effect on brain tissue. This is thought to have the largest impact on brain injury and delayed recovery. Brain stimulation that is inappropriate or excessive can continually over-produce these toxic neurochemical imbalances, causing chronic damage to the brain.
Additionally:
A loss of consciousness does not always occur with a concussion. In fact, a loss of consciousness (if less than 30 minutes) does not even predict how severe the symptoms of a concussion will be.
Injuries to the brain can be focal (only a specific area affected) or diffuse (multiple areas affected). In most cases, concussions damage many regions of the brain (4).
Current research divides concussion into the following 7 categories of injuries:
1) Cognitive – difficulty with memory, speech, complex thought, multi-tasking
2) Oculomotor – issues with eye movement control
3) Affect/Emotional – responding inappropriately to emotional triggers
4) Cervical Spine – pain or movement issues of the neck
5) Headache – localized or general, constant or intermittent
6) Cardiovascular – heart rate & blood pressure control and coordination
7) Vestibular – problems with reactions to changes in head motion and position
Post Concussion Symptoms
Concussion symptoms can appear immediately, within the same day as the injury, or in some cases can present themselves days or weeks following a concussion. The symptoms that are delayed in onset usually become the primary symptoms as an initial Concussion transitions to Post-Concussion Syndrome.
The most common symptoms of post concussion syndrome:
PHYSICAL
Headache (migraine, tension, post-traumatic and cervicogenic)
Nausea/vomiting
Dizziness/Vertigo
Vision problems (e.g. blurring, double or shaky vision)
Light sensitivity (including difficulty looking at computer / TV screens)
Tinnitus (ringing in the ears)
Difficulty sleeping
Fatigue
Neck pain and movement stiffness
COGNITIVE
Difficulty concentrating (brain fog)
Memory loss
Slow or inaccurate speech
Problems with multi-tasking
Difficulty reading
PSYCHOLOGICAL
Anxiety
Depression
Irritable and irrational moods
Impulsive behavior
Difficulty maintaining relationships with partner, family, friends, colleagues
How is Post Concussion Syndrome Diagnosed?
Diagnosis of PCS is typically done by reviewing the patient’s history, physical tests, manual neurological and visual testing, vestibular tests, and ruling out other possible conditions. Here are some details of the most common post-concussion syndrome assessments.
Patient History
- How did the concussion occur?
- When did the symptoms start and how have they changed since then?
- If there was a loss of consciousness, for how long?
- Engage in a Dark Room Protocol or did you continue with all of your usual activities?
- Prior concussions and details?
- Other medical issues?
- What tests/exams have been conducted so far?
- What treatments have you tried or are currently undergoing?
Central Neurological Exam
- Tests for Cerebellar brain function
- Tests for Upper Motor Neuron function
- Cranial Nerve tests
Oculomotor Vision Tests
- Smooth Pursuit
- Saccades
- Convergence and Divergence
Orthopaedic / Physical Exam
- Cervical spine (neck) assessment
- Range of motion
- Strength
- Joint stability
- Treadmill cardiovascular stress testing
- Heart rate / blood pressure tests
Vestibular Tests
- Vestibular Ocular Reflex (VOR) tests
- Positional tests for BPPV
- Gait and Balance Assessments
- Infrared Goggle Nystagmus Tests
Nystagmus refers to the reflexive eye movements that occur with head movement and position changes. Abnormal nystagmus can be a sign of a vestibular impairment (the head movement sensing system), cerebellar and brain stem problems, and vision processing disorders. Nystagmus appears as repetitive flicking or beating movements of the eye (up, down, sideways and rotational).
Infrared google tests assess these patterns of eye movements to determine which areas of the brain may not be functioning properly.
SCAT-5?
The Sideline Concussion Assessment Tool is the most commonly administered test for sports related concussion. However this is a screening test rather than a true diagnostic test and it’s designed to be used for sports injuries and immediately following a concussion. It’s usefulness as a concussion test decreases as time passes, losing effectiveness in as little as 3 days (5) . It is NOT typically used for diagnosing Post-Concussion Syndrome.
X-Rays
Though uncommon, a small number of patients may have serious structural injuries to their neck (cervical spine) with a concussion. Those with significant neck pain, substantial loss of range of motion, or specific neurological signs may benefit from an X-ray.
MRI or CT Scans
The majority of MRIs and CT scans are negative for those with post concussion syndrome (6). In those uncommon cases where head scans show changes in structure or scarring related to a brain injury, this information rarely helps to guide treatment. This is due to the individual differences between patients, and the unique brain stimulation that each person is exposed to each day. However, research in this area is moving quickly and there is strong potential for brain scans to be helpful in the assessment and treatment of PCS in the future.
When is an MRI / CT Scan useful?
- They have little value when symptoms are relatively stable
- Are important if symptoms are rapidly increasing in the initial 3 days of concussion injury. Some worsening signs include: trouble speaking, difficulty coordinating movements of hands, fingers, feet, legs, unbearable headache, persistent vomiting, vision loss.
- If severe symptoms persist well into weeks and months, to rule out a chronic subdermal hematoma (slow brain bleed).
Post Concussion Treatment
Early in the 20th century, concussions were though of as minor issues and were assumed to heal on their own. Then as concussions became recognized as legitimate disorders, post-concussion symptoms were treated with rest and monitoring, and patients may have been given generic written guides to follow. However, there has been growing evidence that this approach can actually prolong recovery and patients may be left with long term brain impairments and concussion symptoms (7) (8) (9).
In response, the medical community has been gradually changing how they view concussion recovery. Current best-practice recommendations include early treatment that encourages activity and appropriate brain stimulation through specific exercise prescription. Guidance from a qualified concussion therapist, such as a vestibular physiotherapist, is recommended.
Recovery can occur through 2 main processes:
1) healing of the damaged nerve cells (usually in the early phase)
2) undamaged neurons compensating for the damaged areas (usually in the later phases) – i.e. neuroplasticity
Is there a specific concussion treatment protocol to follow?
The simple answer is no.
The brain is an extremely complex system and injuries usually result in varied and complex presentations. This means that every patient’s injury is different and each requires specific treatment strategies.
Healing very much depends on how the brain is stimulated throughout the recovery process. Since no two person’s jobs, roles, goals and lives are the same, the types and patterns of brain stimulation is different for everyone.
Therefore the most appropriate treatment strategies adapt to the patient’s symptom patterns day by day, week by week. Skilled concussion therapists will continually monitor and recognize the effects of these symptom changes and make changes to your treatment protocol to optimize your recovery.
In simplest terms, recovery from post concussion syndrome requires 3 factors:
1) limit exposure to inappropriate or excessive “bad” stimulation
2) increase or repeat exposure to “good” stimulation
3) time
Your concussion therapist will assess you and continually reassess you to help guide you through this process. They will identify the “bad” stimuli and “good” stimuli based on your specific concussion impairments. Then create a program for you to follow that adapts and changes with your progress over time.
Understanding Brain Stimulation
Stimulation comes in all forms and sizes. Any activity that causes a brain cell to “fire” causes stimulation.
This chart has specific examples of stimulation and some values that estimate how much brain stimulation they create. Note: the “Amount of Stimulation” column are made up values to help demonstrate this concept.
Cognitive Load is the sum of all of the stimulation that your brain is exposed to at any given time.
We all have an upper limit to how much Cognitive Load we can tolerate. If you exceed it, your brain starts to function less efficiently. Post concussion syndrome means you have a much lower limit to your Cognitive Load threshold. Therefore, it takes very little stimulation to exceed it, resulting in an increase in symptoms. If Cognitive Load remains higher than your threshold for long periods of time, your recovery can stop or even move backwards.
Properly balancing brain stimulation and Cognitive Load is critical to optimizing recovery from PCS.
Rest (the wait and watch method)
Rest has a critical role in concussion recovery, particularly in the first few days, OR if the concussion injury is significant. Rest allows the damaged areas of the brain to be shielded from over-stimulation, preventing a further worsening of the condition. Some patients (but not the majority) may be advised to undergo a “dark room protocol” when they spend a prescribed period of time in a quiet, dark place with little exposure to sound, light, people, and activity.
Rest is often over-prescribed and newer studies show that for moderate or milder concussions, too much rest can actually delay recovery or promote inappropriate healing of the brain, which can lead to chronic, long-term impairments (10). The “wait and watch” method should not be the primary focus of recovery from post concussion syndrome.
Patient Education
Much of the early phases of rehabilitation is spent guiding and teaching the patient about their injury and how to navigate the confusing do’s and don’ts as they work through recovery. These include:
- What types of activities to avoid throughout the healing process
- When to introduce different types of stimulus back into the daily routine
- A framework for return to sport and physical activity
- Creating a modified and gradual return to work schedule
- Advice on alcohol, hydration, diet and other lifestyle factors
Orthopaedic Physiotherapy
Experienced physiotherapists can assess and treat patients who require help in this area. This includes targeted manual therapy techniques to improve motion and reduce pain, as well as physical therapy exercises to improve core strength, stability, and functional movement patterns. Orthopaedic physiotherapy is also effective for reducing Post Concussion Headaches symptoms.
Studies show that vestibular rehabilitation combined with physiotherapy treatment directed at the neck, significantly reduces post-concussion recovery time (11).
Vestibular and Concussion Exercises
Vestibular physiotherapists typically guide patients through a progressive exercise program targeting each patient’s specific impairments. These commonly include:
- Visual gaze stabilization exercises
- Proprioception (awareness of head and body position)
- Motion desensitization
- BPPV correction
- Balance retraining
- Oculomotor exercises (convergence, smooth pursuit, saccades)
- Gait and movement coordination
- Multi-sensory integration
- Graded aerobic training and submaximal heart rate exercise prescription
As 81% of new concussion patients have a vestibular dysfunction this area of rehabilitation is a cornerstone of the recovery process (12).
Learn more about Vestibular Rehabilitation Therapy here.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy involves guidance from a social worker or psychologist with experience in the management of the stress, anxiety and psychosocial aspects of post concussion syndrome. Patients learn strategies to better cope with these issues and get help with difficulties in their transition back to work or school.
Medication
At this time, there are no specific guidelines for concussion medication prescriptions. Pharmaceuticals are prescribed on an individual basis depending on the patient and their physician or specialist.
Common medications include:
- NSAIDs (anti-inflammatories like ibuprofen or naproxen)
- Analgesics (pain reducers like Tylenol)
- Anti-Depressants (SSRIs, amitryptiline)
- Amantadine (increases dopamine)
- Botox injections
- Nutritional Supplements and Vitamins
Vision Therapy
Vision therapy can help with addressing more significant visual complaints. This is commonly done by optometrists with specialized vision therapy credentials. Common strategies include vision exercises, prism lenses, and updating glasses/contact lens prescriptions.
How Long Does Concussion Syndrome last?
Symptoms from post-concussion syndrome can resolve in just a few weeks or can persist for years. In some severe cases, concussion impairments can be permanent. 75% of PCS patients will find their symptoms resolve within 6 months. The majority of the other 25% will resolve within 2 years, and a smaller proportion will continue to experience symptoms after this mark. One recent study found that average post-concussion patient’s symptoms lasts for 7 months. (13)
Risk Factors for Longer Recovery from Post Concussion Syndrome:
- History of previous concussions (the greater the number and severity = longer recovery time) (14)
- Loss of consciousness > 30 min at time of injury
- Anxiety and Depression syndromes
- Females > males
- Adolescents > Adults
- ADHD (attention deficit hyperactivity disorder)
- History of Migraines
- Lack of participation in an active rehabilitation program
- Inability to limit over-stimulation during recovery (premature return to work, sport)
Patterns of Recovery from PCS
There is no test, tool or concussion specialist that can accurately predict when you will be fully recovered. However, we do know that the vast majority of patients eventually get better.
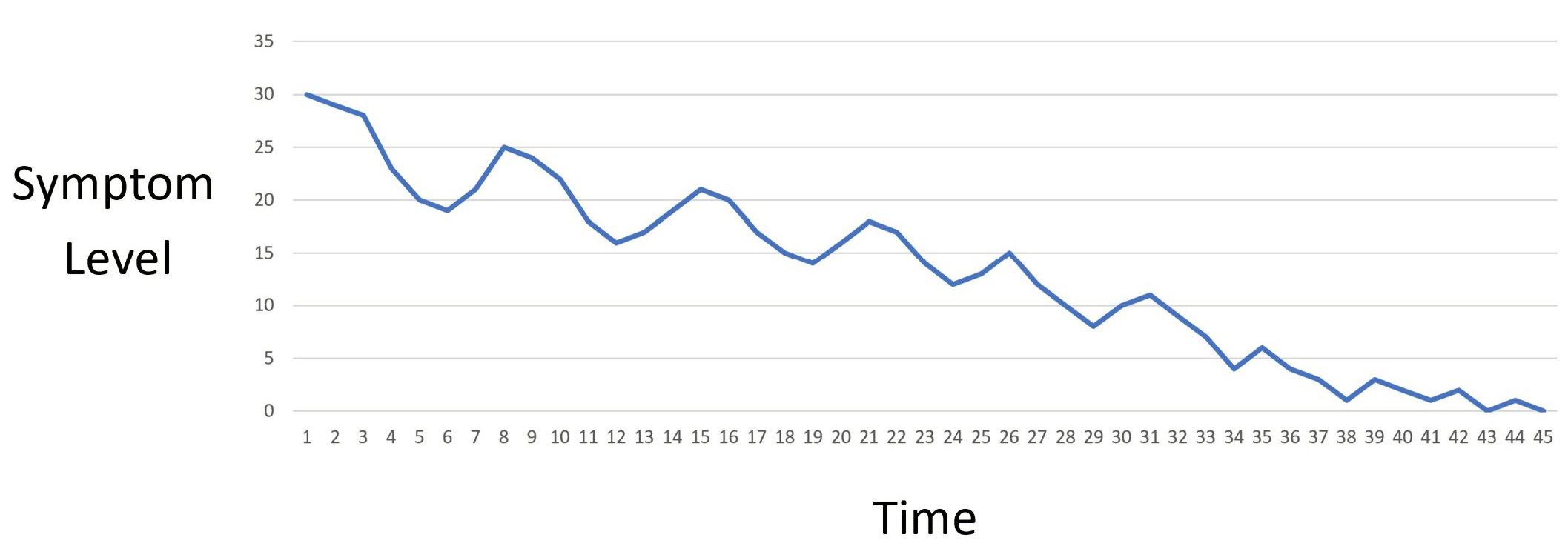
Your symptoms generally follow an up and down fluctuation throughout the entire process.
Your recovery will go through periods of improvement and regression. You’ll notice a few weeks of regular progress then periods of time where your symptoms flare up. This is due to the fact that the amount and pattern of brain stimulation you expose yourself to is not constant and varies from day to day. This is normal. In fact, patients who don’t experience this up/down fluctuation are likely not doing enough to give their brains the stimulation they need.
Can post concussion syndrome come back?
As mentioned earlier, the primary way that your brain recovers from post concussion syndrome is through neuroplasticity. Here, the undamaged neurons in your brain help out, or take over, functions from the damaged neurons. This neuroplasticity is a dynamic, ongoing process that can be affected by many different factors.
Here are some examples of factors that can have a negative effect on neuroplasticity:
- Unmanaged anxiety and depression
- Episodes of high levels of stress (particularly when coping mechanisms are poor)
- Poor lifestyle choices (alcohol, drug use, smoking, poor diet)
- Change in medical health history (cardiovascular and circulatory issues, neurological conditions, hormonal imbalances, new migraine, vision-related, or vestibular diagnoses)
For many patients, keeping post concussion symptoms away, can be achieved by managing these types of factors that can disrupt neuroplasticity and brain compensation.
Also note, that once you’ve had a concussion, you’re 3 times more likely to experience another concussion than someone who hasn’t. (15)
Post Concussion Treatment Near Me
The Cornerstone Dizziness Clinics provide treatment for those suffering from post-concussion syndrome, by registered physiotherapists experienced in traumatic brain injury management. Cornerstone Physiotherapy has clinic locations in downtown and midtown Toronto, North York, Markham and Burlington.
We can also provide consultations through virtual therapy sessions or a mix of in-clinic and remote physiotherapy. Call us today and get us on your team. Contact us here.
REFERENCES:
- C.N. Bennett, R.K. Gupta, P. Prabhakar, R. Christopher, S. Sampath, K. Thennarasu, training in traumatic brain injury in the context of spontaneous recovery, Clinical EEG Neurosci. 49 (2018) 433–440Rajeswaran, Clinical and biochemical outcomes following EEG neurofeedback
- Centers for Disease Control and Prevention, Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2014 (Accessed 10 November 2019).
- Whiteneck GG, Cuthbert JP, Corrigan JD, Bogner JA. Risk of negative outcomes after traumatic brain injury: a statewide population-based survey. J Head Trauma Rehabil 2016;31:E43-54.
- Lux WE. A neuropsychiatric perspective on traumatic brain injury. JRRD 2007;44(7):951-962.
- Lumbabrown, A.; Teramoto, M.; Bloom, O.J.; Brody, D.L.; Chesnutt, J.C.; Clugston, J.R.; Collins, M.W.; Gioia, G.A.; Kontos, A.P.; Lal, A.; et al. Concussion Guidelines Step 2: Evidence for Subtype Classification. Neurosurgery 2020, 86, 2–13.
- Borg J, Holm L, Cassidy JD, Peloso PM, Carroll LJ, von Holst H, et al. Diagnostic procedures in mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med 2004; 36 (suppl 43): 61-75.
- McMahon P, Hricik A, Yue JK, et al. Symptomatology and functional outcome in mild traumatic brain injury: results from the prospective TRACK-TBI study. J Neurotrauma 2014;31:26-33.
- Theadom A, Barker-Collo S, Jones K, et al. Work limitations 4 years after mild traumatic brain injury: a cohort study. Arch Phys Med Rehabil 2017;98:1560-6.
- de Koning ME, Scheenen ME, van der Horn HJ, et al. Non-hospitalized patients with mild traumatic brain injury: the forgotten minority. J Neurotrauma 2017;34:257-61.
- K.G. Harmon, J.R. Clugston, K. Dec, B. Hainline, S.A. Herring, S. Kane, A.P. Kontos, J.J. Leddy, M.A. McCrea, S.K. Poddar, M. Putukian, J.C. Wilson, W.O. Roberts, American Medical Society for Sports Medicine position statement on concussion in sport, Br. J. Sports Med. 53 (2019) 213–225
- Schneider, K.J.; Meeuwisse, W.H.; Nettelaguirre, A.; Barlow, K.M.; Boyd, L.A.; Kang, J.; Emery, C.A. Cervicovestibular rehabilitation in sport-related concussion: A randomised controlled trial. Br. J. Sports Med. 2014, 48, 1294–1298.
- Corwin, D.J.; Wiebe, D.J.; Zonfrillo, M.R.; Grady, M.F.; Robinson, R.L.; Goodman, A.; Master, C.L. Vestibular Deficits following Youth Concussion. J. Pediatr. 2015, 166, 1221–1225.
- Tator CH, Davis HS, Dufort PA, Tartaglia MC, Davis KD, Ebraheem A, Hiploylee C. Postconcussion syndrome: demographics and predictors in 221 patients. J Neurosurg. 2016 Nov;125(5):1206-1216.
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, Kutcher JS, Pana A, Putukian M, Roberts WO. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013 Jan;47(1):15-26.
- Centers for Disease Control and Prevention Guideline on the Diagnosis and Management of Mild Traumatic Brain Injury Among Children. JAMA Pediatr. 2018;172(11):e182853. doi:10.1001/jamapediatrics.2018.2853

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749