Call Us
by Joon Nah
updated Jan 8, 2021
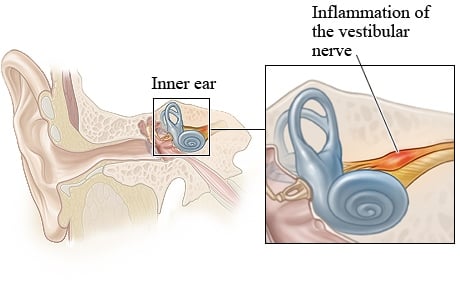
Vestibular neuritis (or vestibular neuronitis) is a neurological condition resulting from an inflammation of the nerve(s) of the inner ear, and can produce dizziness, imbalance, motion sensitivity, nausea, and visual problems. It is the third most common cause of vestibular disorders and can result in mild symptoms or can result in severe difficulty with regular activities of daily living.
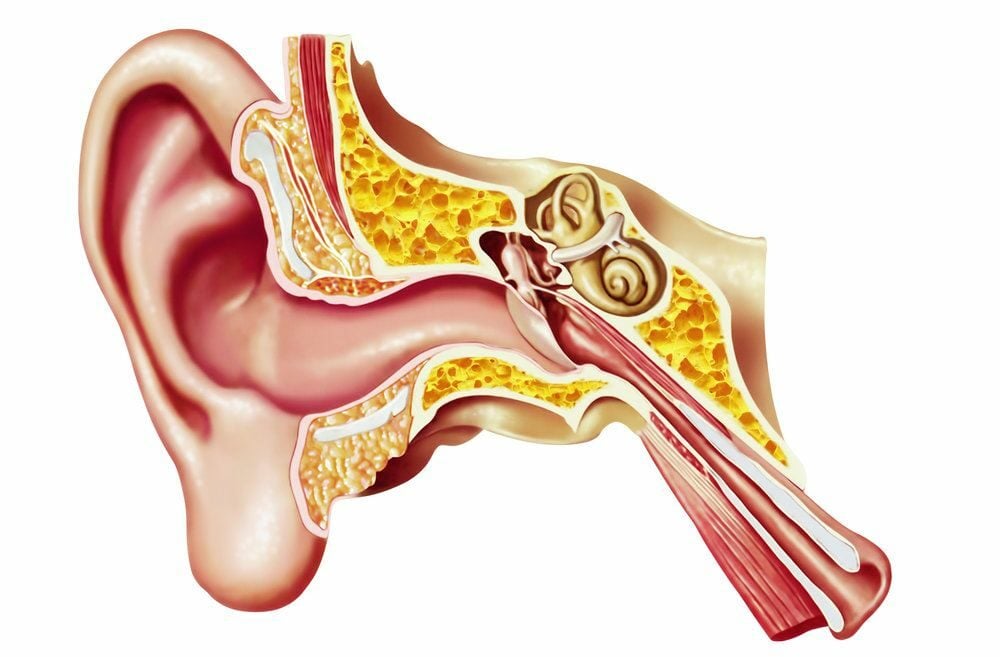
Your vestibular system helps you sense motion and position and allows you to react to these sensations through reflexes in your trunk, legs and arms and eyes. It is made up of the vestibular organ in your inner ear (the sensor), your brain (the processor) and the vestibular nerve (the link between the ear and the brain).
Learn about the causes, diagnosis, treatment and prognosis of vestibular neuritis below.
Vestibular Neuritis Vs Labyrinthitis
Vestibular neuritis and vestibular labyrinthitis are two different conditions that are often mistakenly thought of as the same. With neuritis, only the vestibular nerve is affected whereas labyrinthitis results from damage to BOTH the vestibular nerve and the cochlear nerve (auditory nerve). Therefore vestibular labyrinthitis results in additional symptoms related to hearing loss and/or tinnitus.
Symptoms of Vestibular Neuritis
Vestibular neuritis generally involves and acute phase and a post-acute (chronic) phase. The initial phase lasts between 2 days to 1 week, and the post-acute phase can last weeks, months, or result in long-term symptoms.
INITIAL (ACUTE) PHASE
- Typically a sudden onset of rotational vertigo
- Nausea, vomiting
- Significant imbalance and difficulty walking
- Visual issues with focusing, and tracking of objects
- Severe motion sensitivity
POST-ACUTE PHASE
- General dizziness and light-headedness
- Milder nausea
- Imbalance and difficulty walking in busy environments
- Motion sensitivity with quick head movements
- Visual issues with tracking of objects, screens, busy visual environments
- Ear fullness in some cases
- Anxiety
Symptoms can vary greatly between patients and between cases. This is due to the variety of different causes, the potential for different parts of the nerve affected, and pre-existing conditions or a history of previous dizziness.
Can vestibular neuritis cause headaches?
Some patients can experience the onset of, or an increase in headaches. This can be related to the strain on the head and brain as it struggles to deal with the excessive symptom load it is subjected to. It may also be related to the strain on the upper neck that often accompanies significant dizziness that creates referral pain into the head (cervicogenic headaches).
What Causes Vestibular Neuritis?
Current research is leading us to believe that the most common cause of vestibular neuritis is from a viral infection of the inner ear. The damage we see to the vestibular nerve is similar to that we see from the herpes zoster virus (1). Other causes can include local blood clots (a thrombosis), and auto-immune deficiencies.
These triggers create an inflammatory process at the level of the vestibular nerve which results in a reduction in local blood flow and damages vestibular nerve cells. This initial inflammation produces the much more intense Acute Phase symptoms noted above. Then after a few days, as the inflammation subsides, the resultant local vestibular nerve damage produces the post-acute symptoms.
Vestibular neuritis, is it contagious?
Viruses are passed from person to person therefore technically, someone with vestibular neuritis would have “caught it” from a passed along viral infection. However the condition “vestibular neuritis” itself is not contagious, and you shouldn’t worry that someone suffering from the symptoms of this condition would pass those symptoms on to you.
Why am I dizzy?
The vestibular nerve communicates messages about head position and motion from your inner ear to your brain. When this nerve is damaged, these messages become jumbled and inaccurate, confusing your brain and producing the dizziness, nausea and movement issues.
What are the Risk Factors for Vestibular Neuritis?
- Usually between the ages of 30-60 with most between 40 and 50.
- Affects males and females at the same rate
- 30% have common colds just prior to their dizziness symptoms
Click here for other Common Causes of Dizziness
How is Vestibular Neuritis Diagnosed?
There is no specific test or scan that accurately diagnoses vestibular neuritis. Diagnosis is dependent on a combination of factors that rule it in, and those that rule it out.
Some of these diagnostic factors include:
- History – what specific symptoms and in what pattern did they onset? e.g. if you repeatedly suffer intense episodes of vertigo (after the initial acute phase), you likely do NOT have vestibular neuritis
- Manual neurological tests – that look at vestibular function and rule out other neurological causes
- Balance and gait testing – do they match the suspected loss of vestibular function?
- Nystagmus – are there errors in vestibular eye reflexes? And do they match the patterns associated with a vestibular neuritis?
- Positional tests – do the symptoms and nystagmus patterns match a vestibular neuritis or correlate to other vestibular problems, or to non-vestibular causes?
- Caloric tests – do warm/cold water or air injections into the inner ear register changes in vestibular nerve function?
Skilled vestibular physiotherapists can assess the vestibular system and help arrive at an appropriate diagnosis, including whether you have vestibular neuritis.
Does vestibular neuritis show up on MRI?
No. The damage from vestibular neuritis occurs at the level of nerves and neural cells. MRI tests or CT scans do not have the resolution to show this level of detail.
Vestibular neuritis vs BPPV
The dislodged crystal particles associated with BPPV (benign paroxysmal positional vertigo) is the most common inner ear disorder, therefore vestibular neuritis often gets confused for this condition. BPPV (a mechanical disorder) causes rotational vertigo with very specific head positions where vestibular neuritis (a neurological disorder) is less position dependent and has a much wider range of symptoms.
Learn more about BPPV here.
VESTIBULAR NEURITIS TREATMENT
1. Vestibular Suppressant Medication
These are often prescribed, with the most common in Canada being Serc (betahistine dihydrochloride) and Gravol (dimenhydrinate). These drugs do not actually “cure” the disease, rather attempt to reduce the symptoms related to it (think of taking Tylenol for a sprained ankle).
However Serc particularly, as a vestibular suppressant, has its best effects in the acute phase (first few days) when the vestibular system is hyper-active. After this period of time, its effectiveness is quite limited and in many cases can actually interfere with your head’s ability to compensate, resulting in long term dizziness problems.
We advise you speak with your physician or pharmacist about how using Betahistine and whether they have concerns over long-term usage.
2. Corticosteroid Therapy
Steroid-based medications such as methylprednisolone and glucocorticoids have been shown to help with reducing the length of the acute phase of neuritis by increasing the speed of vestibular compensation. These steroids work to reduce inflammation of the vestibular nerve and decrease direct damage to the nerve itself. However, they are best taken within the first week of the onset of symptoms, when there is active inflammation more likely to be present. Seek an appointment with your physician or to an urgent care center.
3. Vestibular Physiotherapy
Vestibular rehabilitation is regarded as the primary treatment for vestibular neuritis. Studies have shown excellent results related to physical therapy treatment (Vestibular Rehabilitation Therapy – VRT). Physiotherapy identifies the specific problems related to the affected vestibular organ (as this is usually unique to each patient) then uses vestibular rehabilitation exercises to improve compensation gradually reducing the symptoms.
Exercises can involve components of gaze (eye/head) stabilization, balance, desensitizing head/body movements, proprioception (positional awareness), visual tracking and more.
Learn more about Vestibular Rehabilitation here
VESTIBULAR NEURITIS PROGNOSIS
Will vestibular neuritis go away? If so, when?
The good news is that the severe vertigo and symptoms that occur at the Acute Stage of onset improves significantly over the first 1-3 days. And many patients (50%) can feel symptom-free in up to 6 weeks after the onset of symptoms.
However, there is a substantial proportion of people that don’t achieve the vestibular compensation to feel adequately recovered from their vestibular neuritis. These patients often mistakenly believe they are feeling much better, where in reality they have been (consciously or sub-consciously) avoiding the motions and activities that trigger their symptoms.
Our Dizziness Clinics have found:
1) The longer you wait to treat your condition, the longer it takes to get better. Neuro-plasticity gains permanence with time and repetition.
2) No matter how long symptoms have been present, every patient has the ability to achieve some level of improvement. Anywhere from partial recovery to the complete absence of symptoms.
Additional Risks
10-15% of patients develop BPPV in the affected ear within a few weeks (1)
Can vestibular neuritis recur?
Studies show as little as 1.9% of cases of vestibular neuritis can truly reoccur.
However the symptoms from a single case of vestibular neuritis can last for years with fluctuations and symptoms coming and going being a common presentation.
Link Between Vestibular Neuritis and Covid-19?
Covid-19 is a condition that affects blood flow through thromboembolic effects which can cause damage to neural tissue throughout the body, including vestibular pathways. Case studies are already emerging that are implicating the novel coronavirus as the cause of vestibular neuritis in patients. http://europepmc.org/article/MED/32760619
We will continue to update our content as we gain more credible information about the connection between Covid-19 and vestibular dysfunction.
We Can Help.
Cornerstone has Dizziness Clinics in Toronto, North York and Burlington. We have been providing vestibular rehabilitation since 2008 and are close partners with our local medical communities.
Click here to learn how we can help you.
References:
(1) Strupp, M., & Brandt, T. (2009). Vestibular Neuritis. Seminars in Neurology, 29(05), 509–519. doi: 10.1055/s-0029-1241040
Joon Nah BScPT
Certified Vestibular Physiotherapist
Joon is the co-founder of the well-known Cornerstone Dizziness Clinics located in Burlington, North York and Toronto. He received his certificate in Vestibular Rehabilitation from the Emory School of Medicine and is both a clinician and educator in his specialized field.
Learn more about Joon here.

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749