Call Us
by Courtney Steele MScPT
Pelvic Physiotherapist
updated Feb 24, 2022
Everybody poops! But does everybody talk about it? No!
It is so important for our health and overall wellbeing to move our bowels regularly and with ease. Hopefully this article will help shed some light on effective strategies if you are struggling with bowel movements.
Most people don’t realize pelvic floor physiotherapists can help in this area but , speaking as a pelvic physiotherapist, it’s something we see quite often and it’s associated with many conditions we treat.
Generally speaking, you are considered constipated if you are having uncomfortable or infrequent poops. Your colon’s main job is to absorb water from residual food as it moves through your digestive system. It then creates stool. The colon’s muscles propel the waste out through the rectum to be eliminated. If stool remains in the colon too long, it can become hard and difficult to pass (constipation).
What are the signs/symptoms of chronic constipation?
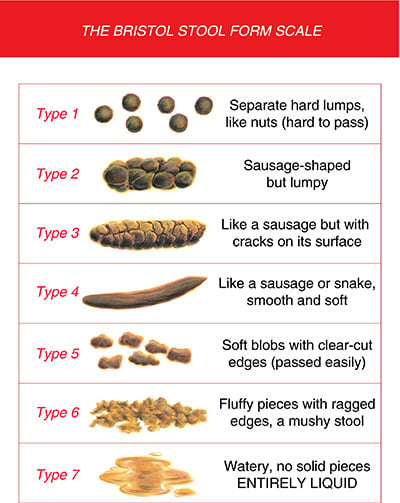
There are a few things to consider when trying to determine if you are constipated. It is not just about the frequency of your bowel movements (BM) – you can have a BM every day and still be constipated!! You need to consider what the BM looks like (see Bristol stool chart below), the time it takes to pass and if straining is involved.
Generally you are considered constipated if you have one of the following:
1) You have fewer than three bowel movements per week
We all poop at different frequencies, but the accepted definition of constipation is two bowel movements per week or fewer. Regular bowel movements are a sign of good digestive health.
2) When you are not type #3 or #4 on the Bristol stool chart
Don’t be shy to look – it’s important! Even if you are type 6/7 you could still be constipated – the loose stool may be all that can make it out – it is leaking around the blockage in your rectum or intestine. Note, Type 3 &4 are considered normal. Type 2 means constipated and Type 1 means very constipated.
3) Straining
If you have difficulty passing a bowel movement, if you’re holding your breath when pushing, and if you’re taking longer than five minutes to pass stool, you are straining.
4) Feeling like you are not fully emptying
Feeling like you didn’t get it all out when you do have a BM. If this is happening it can lead to constipation symptoms like bloating or abdominal discomfort from stool being stuck in the rectum or intestine.
Why Does Constipation Occur?
Constipation most commonly occurs when waste/stool moves too slowly through the digestive tract or cannot be eliminated effectively from the rectum, which may cause the stool to become hard and dry. There are many different factors that can affect why you are constipated, such as:
1) Conditions that affect hormones:
- Underactive thyroid (hypothyroidism)
- Diabetes
- Menstrual cycle – more BM issues around ovulation (before period comes) due to changes in hormones
- Pregnancy – hormone related as well as a little baby taking all the nutrients they need as well as growing inside the uterus which squishes the intestines, slowing motility through your gut leading to constipation.
2) Delaying your poop
Don’t ignore the urge! Unlike the urge to pee, you can ignore the urge to poo. If you do, this signal will usually go away. However, by doing this the stool stays in your colon longer, meaning more water is getting pulled out and the stool is getting harder and thus more difficult to pass. This can lead to a build up of stool/bloating/abdominal pain.
3) Outlet dysfunction/dyssynergia
Pelvic floor muscles that don’t coordinate properly to allow for the expulsion of stool.
4) Sedentary lifestyle
5) Older age
6) Neurological problems
This can affect the nerves that cause muscles in the colon and rectum to contract and move stool through the intestines. Examples include: Multiple sclerosis, Parkinson’s disease, spinal cord injury and stroke
7) Rectocele (type of prolapse)
8) Megarectum or hyposensitive rectum
9) Stenosis of internal anal sphincter (i.e. Crohn’s)
10) Medications
Certain medications can cause constipation including sedatives, opioid pain medications, some antidepressants or medications to lower blood pressure.
11) Traveling
The gut is a creature of habit (aren’t we all?!). The nerves of the gut remember what type of food we eat, when we eat it, whether it is night or day and what time we usually go to the washroom. When we travel (especially if changing time zones) we suddenly change all these familiar patterns/routines. We are eating processed foods, drinking less water, dealing with jetlag and the nerves of the gut get confused, throwing off our regular bowel movements.
To help with this, start eating high fiber foods the day before or day of your trip (only add 2-5grams of fiber more than you are used to as otherwise you might have trouble digesting it and get gassy). It can take a few days for our body to feel the effects of a fiber increase so plan accordingly.
12) Mental health conditions
Yes – depression, anxiety and chronic stress can all cause constipation. When your nervous system is in flight or flight mode (i.e. in chronic stress) it slows the contractions of the gut – your body is not focused on digestion. An analogy I use to describe this to my patients is to think about if you were under a physical stressor – let’s say you really had to go the the bathroom, then you realized your house was on fire…you would no longer feel the urge to go – your body is activating the muscles to help you get to safety it is not focused on having a BM in that moment!
Emotional stressors work the same way on our nervous system – causing digestion to slow down, stool to sit in your intestine which then dehydrates and this can lead to constipation.
Stress also causes us to hold tension in our muscles and one of the areas most affected by this believe it or not is your pelvic floor! These muscles need to relax to evacuate a BM so this is yet another way stress can lead to constipation.
13) Eating disorders
14) Irritable bowel syndrome (IBS)
15) Colon cancer
Signs of colon cancer include: a change to your normal bowel routine (frequency/size/shape of stools) and/or rectal bleeding (this can also be caused by fissures or hemorrhoids) or severe pain when passing stool.
How is the pelvic floor related to constipation?
The pelvic floor muscles (including the anal sphincter) are the gatekeepers – they control when things come out (i.e. urine or bowel movements) so that we don’t have accidents. On the other hand, in order to empty properly, they need to relax.
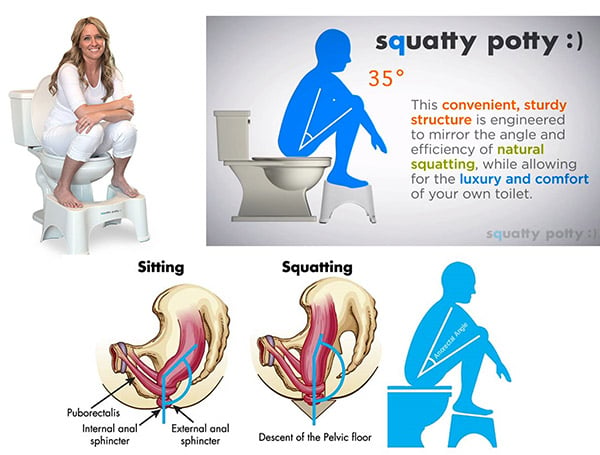
When pelvic floor muscles are tight or hold tension it is hard to pass stool. Think of squeezing a tube of toothpaste with the cap on – you are working hard and straining but are not going to be successful at getting the toothpaste out…this is the analogy I like to use for those of my patients who have a tight pelvic floor or a dyssynergic contraction. Those muscles need to relax for the stool to come out and if they can’t or you are actually contracting them instead you are not going to have a successful BM no matter how much fiber you are eating! This is why we always recommend the squatty potty – see below for more info on this.
How do pelvic floor physiotherapists go about treating constipation?
- Education – more on all the things discussed in this blog
- Performing and teaching the ILU massage
- Fiber diaries – often we ask our patients to fill out a fiber diary to see if they are getting the appropriate amount of dietary fiber and if not help to provide information on how to safely increase this amount in their diet
- Assessment and treatment of the pelvic floor muscles (ensuring proper coordination i.e. pelvic floor muscles are relaxing when bearing down and not contracting, treating tight pelvic floor muscles)
- Biofeedback training
– involves working with a therapist who uses devices to help you learn to relax and tighten the muscles in your pelvis. Relaxing your pelvic floor muscles at the right time during defecation can help you pass stool more easily. During a biofeedback session, a special tube (catheter) to measure muscle tension is inserted into your rectum. The therapist guides you through exercises to alternately relax and tighten your pelvic muscles. This will gauge your muscle tension and helps you understand when you’ve relaxed your muscles.
What other pelvic floor conditions cause constipation?
Constipation is an important factor to consider when patients present with:
- Overactive bladder syndrome
- Anal fissures (tiny tears in the tissue around the anus), hemorrhoids
- Abdominal pain
- Intestinal Obstruction
- Pre-partum – we teach pushing strategies for birth and have our patients practice when having a BM – it’s all the same! Click here to learn how to prepare for childbirth.
- Postpartum – first poops after birth suck! Make them as easy as possible on yourself by using the right set up, eating right and using stool softeners (hint: pack them in your birth bag!). Click here for our guide to recovery after c-section.
- Prolapse
- Urinary incontinence
- Endometriosis
- Pelvic pain
- Fecal incontinence
- Low back pain. Click here for our Guide to the 5 types of low back pain.
Complications of constipation
- Hemorrhoids – straining to have a bowel movement may cause swelling in the veins in and around your anus.
- Anal fissure – a large or hard stool can cause tiny tears in the anus.
- Fecal impaction – chronic constipation may cause an accumulation of hardened stool that gets stuck in your intestines.
- Rectal prolapse – chronic straining to have a bowel movement can cause a small amount of the rectum to stretch and protrude from the anus.
Strategies to avoid constipation
1) Hydration
Most of us don’t drink enough liquid– ideally you should be having around ½ your body weight in liquid (in ounces, keep in mind this counts as anything that is liquid you consume and that means anything that would be liquid at room temperature … the milk in your morning cereal to the ice cream you have for desert). So if you are140lbs… ½ of this is 70lbs = 70oz of liquid a day, a glass of water is approximately 8oz so this equates to 8 glasses of liquid/day. We need good liquid intake to hydrate the stool so it is not hard and it is easy to pass. Liquid also helps improve the speed at which the stool moves through the colon (motility).
2) Movement
Another thing most of us don’t do enough of these days. Physical activity stimulates our gut and helps it to move stool faster. Get moving daily!
3) ILU Massage
If you are constipated, do this daily for 10min in a hot shower or with lotion on your belly. This can really help babies and kids that are backed up too – very soothing and helps to move stool through. Studies show this can help improve frequency of bowel movements.
4) Nutrition
Pelvic floor physiotherapists have a basic knowledge of nutrition and can provide some tips. If you try these tips below and are still struggling it is best you talk to a dietician to get more specific information that is individualized to you and your needs.
- Eat a variety of fiber (soluble and insoluble) – fiber affects the quality of our poops! But make sure you hydrate it! Consuming fiber is of no help if you do not also consume sufficient fluids.
- Insoluble fiber: helps to draw water into our stool (holds water) and helps stimulate movement through the digestive system – important if you know you have slow transit (ex. wheat bran, whole grains, cereals, seeds, and the skins of many fruits and vegetables)
- Soluble fiber: dissolves in water to make gel like substance, making stool softener and easier to deal with ( i.e.dried beans, oats, rice bran, barley, citrus fruits, apples, strawberries, peas, and potatoes)
- All plant foods, including fruits, vegetables, whole grains, and beans, have fiber. Most plant foods contain some of each kind of fiber. Great options for fiber are psyllium seed husks and plums – both contain fiber but also agents that draw extra fluids into the gut – bonus!
- The Academy of Nutrition and Dietetics recommends 25 grams per day for women and 38 grams for men. Eat fruits and veggies with every single meal!
- Some simple ideas to get your fiber
- Breakfast – oats with fruit mixed in, smoothies with veggies/fruits and ground flax or chia seeds (40% fiber), raspberries, blueberries and bananas are really good fiber sources. Add some bran buds or psyllium fiber (remember not too much – don’t want to add fiber too quickly) to your yogurt, cereal or applesauce.
- Lunch ideas – salads – get your leafy greens
- Dinner – ½ or more of your plate is veggies
- See this PDF for a list of foods and their fiber levels (soluble and insoluble)
CLICK TO DOWNLOAD – How to Keep a Fibre Diary – Cornerstone Physiotherapy
- Magnesium citrate
- Minimize alcohol
5) Proper toileting position/habits
Position:
Bowels were meant to move in a squatting position. The key is to get knees higher than hips (i.e use a step stool or a squatty potty under your feet when having a BM). This helps to “unkink” or relax one of the pelvic floor muscles (the puborectalis) that loops/slings around the rectum itself making it easier to empty the rectum. If our knees are not above our hips (how we in western culture tend to toilet) the puborectalis is tight around the rectum causing a kink and making it difficult for anything that is in there to pass easily causing more need for straining.
The squatty potty is a stool specially designed for this as it curves right around your toilet. The squatty potty is famous because of how helpful it is! It has been featured on the popular shows Shark Tank (https://www.youtube.com/watch?v=5ZJkpIm7hmk), the Howard Stern show and in one of my favs – Superstore! (the fact that they featured the squatty potty made me love the show even more than I already do!)
Habits:
Movement on the toilet also helps to encourage stool to pass. Try twisting (twist over your right shoulder with your left hand) on the toilet and doing anterior and posterior pelvic tilts to get things moving vs. straining. Then lean forward and rest your elbows on your thighs. Relax.
Pushing without straining – If you are straining (breath holding when pushing) this tends to tighten the pelvic floor muscles closing off the opening. Make your abdominal muscles bulge outward or make your waist wide with your breath out. Use this movement to push the bowel movement down and out. Blowing into a closed fist can help this bulging, drives pressure down and ensures you aren’t breath holding!
Try this for 5 minutes, if no results, get up and go move around. Try again later when the urge returns. Practice every day as a regular routine is required to help the bowels to move properly. It is a good idea to sit on the toilet for a couple of minutes after every meal to retrain the gastro – colonic reflex. This may take a couple of months to fully re – train but it is worth the effort!
6) Manage stress
7) Don’t ignore the urge to pass stool
8) Try to create a regular schedule for bowel movements
Bowels respond the best to a regular habit – they sleep at night and are active during the day. Food and movement stimulates gut motility you’re most likely to pass a BM is in 30min after the first meal of the day (don’t skip breakfast!). Drinking something warm in the morning can help too.
9) Wear loose clothing
Avoiding clothes that are tight on the waistline or ribcage – these can limit your ability to take big deep breath which helps to relax your pelvic floor. Tight clothing can cause people to suck in or hold tummies in tension, it can lead to a habit of gripping the abdomen and pelvic floor.
10) Probiotics/prebiotics
These supplements can breathe new life into a tired gut. Contact your doctor/pharmacist if you think this might help you to make sure it is right for you.
Most cases of constipation are mild and easily treated with changes in diet and exercise. If you’re experiencing chronic constipation or constipation along with other bowel changes, it’s important that you talk with a healthcare professional. Cornerstone Physiotherapy’s pelvic health program has experienced physiotherapists in Toronto, North York, and Burlington. Call us today – we can help!

Questions? We're happy to help!
Choosing the right service provider can be a big decision. We’re dedicated to answering any questions you have to help you make the best choice. Contact us today and ask us anything!
Call us at (416) 238-6749